The unusual cases of pneumonia began to appear in midwinter, in China. The cause, researchers would later learn, was a coronavirus new to science. By March, the infection began to spread to other Asian countries and overseas. People were dying, and the World Health Organization issued a global health alert.
But this was 2003, not 2020, and the disease was SARS, not Covid-19. By June, the outbreak was almost gone, with just 8,098 confirmed infections and 774 deaths worldwide. No cases of SARS have been reported since 2004.
Contrast that with the closely related coronavirus that causes Covid-19 today: more than 13,600,000 confirmed cases as of July 16, and more than 585,000 deaths.
Why did SARS go away while today’s coronavirus just keeps on spreading? Why, for that matter, did both these coronaviruses spill over into people at all, from their original bat hosts?
And just as vital as those questions is another: What happens next?
As we face the current pandemic, it will be important to understand how SARS-CoV-2, the virus that causes Covid-19, is likely to evolve in the months and years ahead. It’s possible the virus could lose its lethal character and settle into an evolutionary détente with humanity. It might end up as just another cold virus, as may have happened to another coronavirus in the past. But it could also remain a serious threat or perhaps even evolve to become more lethal. The outcome depends on the complex and sometimes subtle interplay of ecological and evolutionary forces that shape how viruses and their hosts respond to one another.
“One thing you learn about evolution is never to generalize,” says Edward Holmes, an evolutionary virologist at the University of Sydney, Australia, and author of an article on the evolution of emerging viruses in the Annual Review of Ecology, Evolution, and Systematics. “It depends entirely on the biological nuance of the situation.”
Steps to viral success
Many of the scariest viruses that have caused past or current epidemics originated in other animals and then jumped to people: HIV from other primates, influenza from birds and pigs, and Ebola probably from bats. So, too, for coronaviruses: The ones behind SARS (severe acute respiratory syndrome), MERS (Middle East respiratory syndrome) and Covid-19 all probably originated in bats and arrived in people via another, stepping-stone species, likely palm civets, camels and possibly pangolins, respectively.
But making the jump from one species to another isn’t easy, because successful viruses have to be tightly adapted to their hosts. To get into a host cell, a molecule on the virus’s surface has to match a receptor on the outside of the cell, like a key fitting into a lock. Once inside the cell, the virus has to evade the cell’s immune defenses and then commandeer the appropriate parts of the host’s biochemistry to churn out new viruses. Any or all of these factors are likely to differ from one host species to another, so viruses will need to change genetically — that is, evolve — in order to set up shop in a new animal.
Host switching actually involves two steps, though these can overlap. First, the virus has to be able to invade the new host’s cells: That’s a minimum requirement for making the host sick. But to become capable of causing epidemics, the virus also has to become infectious — that is, transmissible between individuals — in its new host. That’s what elevates a virus from an occasional nuisance to one capable of causing widespread harm.
SARS-CoV-2 shows these two stages clearly. Compared with the virus in bats, both the virus that infects people and a close relative in pangolins carry a mutation that changes the shape of the surface “spike protein.” The alteration is right at the spot that binds to host cell receptors to let the virus in. This suggests that the mutation first arose either in pangolins or an as yet unidentified species and happened to allow the virus to jump over to people, too.
But SARS-CoV-2 carries other changes in the spike protein that appear to have arisen after it jumped to people, since they don’t occur in the bat or pangolin viruses. One is in a region called the polybasic cleavage site, which is known to make other coronaviruses and flu viruses more infectious. Another appears to make the spike protein less fragile, and in lab experiments with cell cultures, it makes the virus more infectious. The mutation has become more common as the Covid-19 pandemic goes on, which suggests — but does not prove — that it makes the virus more infectious in the real world, too. (Fortunately, though it may increase spread, it doesn’t seem to make people sicker.)
A recent mutation alters the SARS-CoV-2 spike protein to make it less fragile (the altered bits are shown as colored blobs). This added robustness appears to make the virus more infectious. Three sites are shown because the spike protein is composed of three identical subunits that bind together.
This evolutionary two-step — first spillover, then adaptation to the new host — is probably characteristic of most viruses as they shift hosts, says Daniel Streicker, a viral ecologist at the University of Glasgow. If so, emerging viruses probably pass through a “silent period” immediately after a host shift, in which the virus barely scrapes by, teetering on the brink of extinction until it acquires the mutations needed for an epidemic to bloom.
Streicker sees this in studies of rabies in bats — which is a good model for studying the evolution of emerging viruses, he says, since the rabies virus has jumped between different bat species many times. He and his colleagues looked at decades’ worth of genetic sequence data for rabies viruses that had undergone such host shifts. Since larger populations contain more genetic variants than smaller populations do, measuring genetic diversity in their samples enabled the scientists to estimate how widespread the virus was at any given time.
The team found that almost none of the 13 viral strains they studied took off immediately after switching to a new bat species. Instead, the viruses eked out a marginal existence for years to decades before they acquired the mutations — of as yet unknown function — that allowed them to burst out to epidemic levels. Not surprisingly, the viruses that emerged the fastest were those that needed the fewest genetic changes to blossom.
SARS-CoV-2 probably passed through a similar tenuous phase before it acquired the key adaptations that allowed it to flourish, perhaps the mutation to the polybasic cleavage site, perhaps others not yet identified. In any case, says Colin Parrish, a virologist at Cornell University who studies host shifts, “by the time the first person in Wuhan had been identified with coronavirus, it had probably been in people for a while.”
It was our bad luck that SARS-CoV-2 adapted successfully. Many viruses that spill over to humans never do. About 220 to 250 viruses are known to infect people, but only about half are transmissible — many only weakly — from one person to another, says Jemma Geoghegan, an evolutionary virologist at the University of Otago, New Zealand. The rest are dead-end infections. Half is a generous estimate, she adds, since many other spillover events probably fizzle out before they can even be counted.

Funeral for a US soldier who died of influenza in Russia in 1919. The 1918-1920 pandemic killed an estimated 50 million people worldwide.
CREDIT: US NATIONAL ARCHIVES
Getting nicer — or nastier
SARS-CoV-2, of course, is well past the teetering stage. The big question now is: What happens next? One popular theory, endorsed by some experts, is that viruses often start off harming their hosts, but evolve toward a more benign coexistence. After all, many of the viruses we know of that trigger severe problems in a new host species cause mild or no disease in the host they originally came from. And from the virus’s perspective, this theory asserts, hosts that are less sick are more likely to be moving around, meeting others and spreading the infection onward.
“I believe that viruses tend to become less pathogenic,” says Burtram Fielding, a coronavirologist at the University of the Western Cape, South Africa. “The ultimate aim of a pathogen is to reproduce, to make more of itself. Any pathogen that kills the host too fast will not give itself enough time to reproduce.” If SARS-CoV-2 can spread faster and further by killing or severely harming fewer of the people it infects, we might expect that over time, it will become less harmful — or, as virologists term it, less virulent.
This kind of evolutionary gentling may be exactly what happened more than a century ago to one of the other human coronaviruses, known as OC43, Fielding suggests. Today, OC43 is one of four coronaviruses that account for up to a third of cases of the common cold (and perhaps occasionally more severe illness). But Fielding and a few others think it could also have been the virus behind a worldwide pandemic, usually ascribed to influenza, that began in 1890 and killed more than a million people worldwide, including Queen Victoria’s grandson and heir.
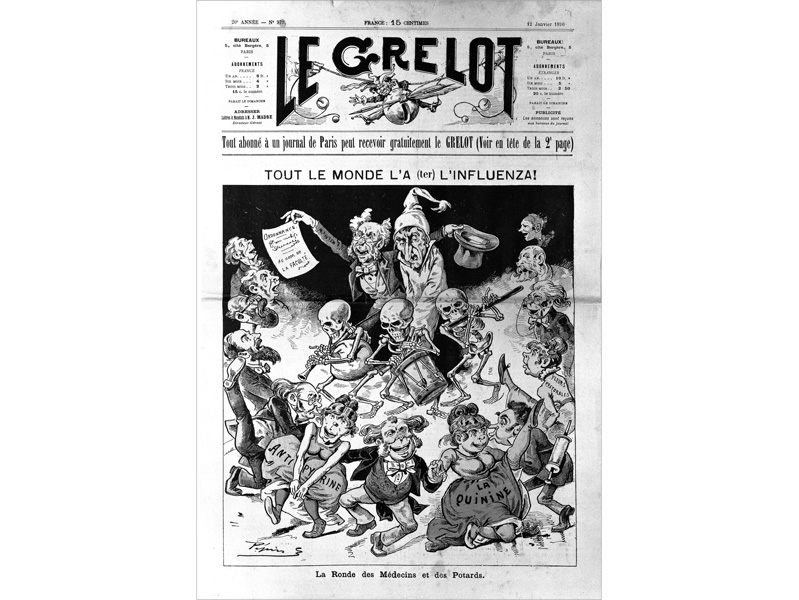
“Everyone has influenza,” says the headline in a French publication from January, 1890.
CREDIT: WELLCOME COLLECTION
Scientists can’t prove that, because no virus samples survive from that pandemic, but some circumstantial evidence makes the case plausible, Fielding says. For one thing, people who were infected in the 1890 pandemic apparently experienced nervous-system symptoms we now see as more typical of coronaviruses than of influenza. And when Belgian researchers sequenced OC43’s genome in 2005 and compared it to other known coronaviruses, they concluded that it likely originated as a cattle virus and may have jumped to people right around 1890. They speculated that it may have caused the 1890 pandemic and then settled down to a less nasty coexistence as an ordinary cold virus.
Other evolutionary biologists disagree. The pandemic certainly faded as more people became immune, but there’s no solid evidence that OC43 itself evolved from highly virulent to mostly benign over the last century, they say. Even if it did, that does not mean SARS-CoV-2 will follow the same trajectory. “You can’t just say it’s going to become nicer, that somehow a well-adapted pathogen doesn’t harm its host. Modern evolutionary biology, and a lot of data, shows that doesn’t have to be true. It can get nicer, and it can get nastier,” says Andrew Read, an evolutionary microbiologist at Penn State University. (Holmes is blunter: “Trying to predict virulence evolution is a mug’s game,” he says.)
To understand why it’s so hard to predict changes in virulence, Read says it’s important to recognize the difference between virulence — that is, how sick a virus makes its host — and its transmissibility, or how easily it passes from one host individual to another. Evolution always favors increased transmissibility, because viruses that spread more easily are evolutionarily fitter — that is, they leave more descendants. But transmissibility and virulence aren’t linked in any dependable way, Read says. Some germs do just fine even if they make you very sick. The bacteria that cause cholera spread through diarrhea, so severe disease is good for them. Malaria and yellow fever, which are transmitted by mosquitos, can spread just fine even from a person at death’s door.
Respiratory viruses, like influenza and the human coronaviruses, need hosts that move around enough to breathe on one another, so extremely high virulence might be detrimental in some cases. But there’s no obvious evolutionary advantage for SARS-CoV-2 to reduce its virulence, because it pays little price for occasionally killing people: It spreads readily from infected people who are not yet feeling sick, and even from those who may never show symptoms of illness. “To be honest, the novel coronavirus is pretty fit already,” Geoghegan says.
Nor are there many documented instances of viruses whose virulence has abated over time. The rare, classic example is the myxoma virus, which was deliberately introduced to Australia in the 1950s from South America to control invasive European rabbits. Within a few decades, the virus evolved to reduce its virulence, albeit only down to 70 to 95 percent lethality from a whopping 99.8 percent. (It has since ticked up again.)
But myxoma stands nearly alone, Parrish says. For instance, he notes, there is no evidence that recent human pathogens such as Ebola, Zika or chikungunya viruses have shown any signs of becoming less pathogenic in the relatively short time since jumping to humans.

After rabbits were introduced to Australia, their population exploded. “They are very plentiful here,” says the handwritten inscription on the back of this postcard from around 1930. Scientists eventually introduced the myxoma virus to control the rabbit plague.
CREDIT: PHOTOGRAPHER PAUL C. NOMCHONG / NATIONAL MUSEUM OF AUSTRALIA
The ones that went away
The faded nightmares of our past — pandemics that terrorized, then receded, such as SARS in 2003 and flu in 1918-20 and again in 1957, 1968 and 2009 — went away not because the viruses evolved to cause milder disease, but for other reasons. In the case of SARS, the virus made people sick enough that health workers were able to contain the disease before it got out of hand. “People who got SARS got very sick, very fast and were easily identified, easily tracked and readily quarantined — and their contacts were also readily identified and quarantined,” says Mark Cameron, an immunologist at Case Western Reserve University in Cleveland, who worked in a Toronto hospital during the height of the SARS outbreak there. That was never going to be as easy to do for Covid-19 because people who don’t show symptoms can spread the virus.
Flu pandemics, meanwhile, have tended to recede for another reason, one that offers more hope in our present moment: Enough of the population eventually becomes immune to slow the virus down. The H1N1 influenza virus that caused the 1918 pandemic continued as the main influenza virus until the 1950s, and its descendants still circulate in the human population. What made the virus such a threat in 1918-20 is that it was novel and people had little immunity. Once much of the population had been exposed to the virus and had developed immunity, the pandemic waned, although the virus persisted at a lower level of infections — as it does to this day. It appears less lethal now largely because older people, who are at greatest risk of dying from influenza, have usually encountered H1N1 influenza or something like it at some point in their lives and retain some degree of immunity, Read says.
With the new coronavirus, Parrish says, “we’re sort of in that 1918 period where the virus is spreading fast in a naive population.” But that will change as more people either catch Covid-19 or are vaccinated (if and when that becomes possible) and develop some level of immunity. “There’s no question that once the population is largely immune, the virus will die down,” Parrish says.
The question is how long that immunity will last: for a lifetime, like smallpox, or just a few years, like flu? In part, that will depend on whether the vaccine induces a permanent antibody response or just a temporary one. But it also depends on whether the virus can change to evade the antibodies generated by the vaccine. Although coronaviruses don’t accumulate mutations as fast as flu viruses, they do still change. And at least one, which causes bronchitis in chickens, has evolved new variants that aren’t covered by previous vaccines. But at this point, no one knows what to expect from SARS-CoV-2.
There is, at least, one encouraging aspect to all this. Even if we can’t predict how the virus will evolve or how it will respond to the coming vaccine, there is something all of us can do to reduce the risk of the virus evolving in dangerous ways. And it doesn’t involve any complicated new behaviors. “Viruses can only evolve if they’re replicating and transmitting,” Streicker says. “Anything that reduces the replication of a virus will in consequence reduce the amount of evolution that happens.” In other words, we can do our part to slow down the evolution of the Covid-19 virus by behaving exactly as we’ve been told to already to avoid catching it: Minimize contact with others, wash your hands and wear a mask.
This article is part of Reset: The Science of Crisis & Recovery, an ongoing series exploring how the world is navigating the coronavirus pandemic, its consequences and the way forward. Reset is supported by a grant from the Alfred P. Sloan Foundation.




