It’s the promise of stem cell medicine: Someday soon, clinics will rebuild diseased or broken hearts, kidneys, pancreases or blood by growing and reprogramming human cells, then adding them back to the bodies of the patients they came from.
If only it were that easy.
After two decades of human stem cell research, researchers have learned how to create what appear to be reasonably functional versions of several types of cells, first using genetic tricks to turn cells back to an uncommitted state and then molding them into the type of cell needed — say, an insulin-producing cell or a particular kind of nerve cell. And many early clinical trials of stem cell medicine have shown genuinely promising results.
But applying such techniques en masse simply won’t be practical, because the lengthy processes for extracting and preparing an individual’s own cells won’t scale up, some scientists say.
For one thing, “everyone’s cells will behave a little bit differently,” says Lonnie Shea, a biomedical engineer at the University of Michigan, Ann Arbor. And then there’s the bottom line. “It is beyond too expensive,” says Douglas Melton, cofounder of the Harvard Stem Cell Institute, a network of more than 1,000 Harvard-affiliated scientists.
Instead, increasingly, labs around the world are seeking to design off-the-shelf cell therapies using universal donor cells that are genetically altered to avoid the many-armed responses of the immune system against foreign tissues. Scientists want to create a suite of such cells tailored for specific tissue repairs: universal muscle cells, universal skin cells or universal insulin-producing pancreatic beta cells.
“The big dream is a cell that would be like a pill, which could go into any patient,” says Melton, who called for a global push to realize this vision at a stem cell meeting in Los Angeles in June.
This trend in regenerative medicine parallels events in cancer medicine. Personalized treatments that genetically reengineer the T cells of patients with certain blood cancers are often effective, but such therapies cost hundreds of thousands of dollars per patient and it can take years for manufacturing to get up and running. Cancer researchers around the world now are working to create off-the-shelf versions.
It’s all part of a broader effort to bring the rapidly advancing power of genetic engineering more deeply into regenerative medicine, says pediatric hematologist Leslie Kean of Harvard Medical School, director of the Stem Cell Transplant Center at Boston Children’s Hospital. “This is not just science fiction anymore.”
Artful dodging
Our bodies normally are quick to reject any cell that isn’t our own. While that response often can be overridden by drugs designed to suppress the immune system, these medicines bring significant risks and side effects. So the goal is for universal donor cells to be “hypoimmunogenic” — able to hold off the immune system’s many lines of defense without requiring immunosuppression.
In one development, scientists at the University of California, San Francisco and colleagues reported in Nature Biotechnology in February that they’d created hypoimmunogenic mouse and human cells through a several-step process. The starting ingredients were iPS cells (induced pluripotent stem cells). These are adult cells engineered to lose their specific cell identities so they can once again become many different cell types, a condition known as pluripotency. By tinkering with a few genes in these iPS cells, the researchers could produce heart cells, muscle cells and endothelial cells (which line the inside of blood vessels). All showed “stealth” behavior to the two main branches of the immune system — adaptive and innate — when transplanted into mice.
To accomplish this, the lab did two things. First, it knocked out several molecules of the human leukocyte antigen (HLA) system — components of the adaptive immune system. The proteins of this system normally stud the surface of cells and signal “otherness” to T cells if they don’t match with the body’s.
“If you take that away, the T cells cannot recognize a cell as foreign, and you don’t see T cell activation anymore,” says Sonja Schrepfer, the study’s senior author and head of UCSF’s Transplant and Stem Cell Immunobiology Lab and a founding scientist for the Seattle-headquartered startup company Sana Biotechnology.
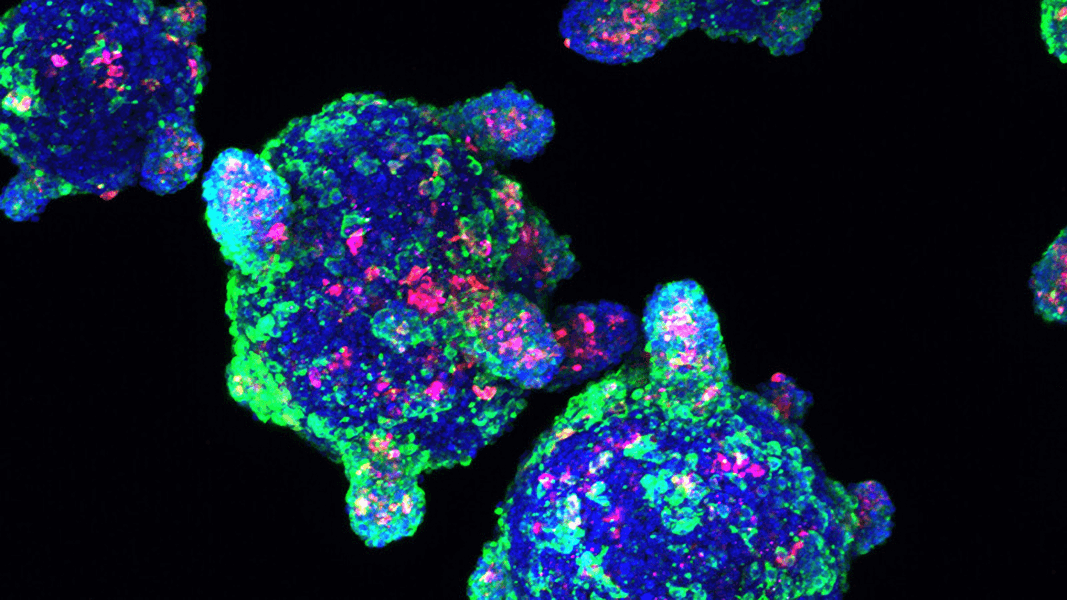
This image shows insulin-producing beta cells that were made from stem cells. Cells like this could one day be transplanted into people with type I diabetes, but they would need to be protected by immune-suppressing drugs or encapsulation. Cost and complexity will remain huge barriers for most therapies based on pluripotent stem cells until scientists can create cells that don’t trigger immune responses.
CREDIT: MELTON LAB / HARVARD UNIVERSITY
But removing HLA activity still leaves other, innate aspects of the immune system intact. For example, natural killer cells will normally wipe out cells that no longer make certain HLA proteins. To solve that problem, Schrepfer and colleagues tapped into a long-studied phenomenon of pregnancy known as fetal-maternal tolerance: why the mother’s immune system will not reject a fetus even though half the proteins are from the father.
The fetus, it turns out, avoids attack by boosting or tamping down the activity of various genes, including one called CD47. And by increasing activity of CD47 as well as removing some HLA molecules, Schrepfer’s team got the results they wanted.
Less is more in modifying iPS cells, Schrepfer says. “Editing of each molecule has risks, so you want to find the minimum combination you need to achieve hypoimmunity.”
Stepping up stealth
Another example of preliminary success with hypoimmunogenic human cells came from a team within the Harvard Stem Cell Institute network, led by stem cell researcher Chad Cowan, now with Sana Biotechnology.
Like the UCSF group, the scientists lowered the activity of certain HLA genes and boosted activity of the CD47 gene in pluripotent cells. But they also increased the production of a different class of HLA molecules: ones that help the fetus dodge the mother’s immune system.
And they added another step, taking lessons learned from cancer cells that evade the immune system. Through genetic tinkering, the team boosted the production of a protein called PD-L1 that these tumor cells use to turn away T cells.
The complex set of genetic modifications, reported in the journal PNAS in April, significantly dialed down immune reaction when the cells were infused in mice. T cell responses were blunted, and attacks by natural killer cells and macrophages (another class of immune cell) were minimal.
Safe housing
As research on universal donor cell therapies moves forward, one of the biggest concerns is that these cells — which are made pluripotent again, then turned into the required adult tissues, using imperfect gene editing tools — may generate tumors. To garner FDA approval, cell lines will have to be extensively vetted for any signs of danger, but there are worries that no process can provide complete protection.
“There are always theoretical concerns about cells retaining some measure of pluripotency, which would mean that they wouldn’t have a signal to stop growing,” says Kean of Boston Children’s Hospital. Still, she says, “there’s been a ton of research to suggest that really won’t be an issue with the iPS-derived cells that are being produced now; a lot of those potential risks have been engineered out.”
Labs also can add an insurance policy in the form of suicide genes, a technique long studied in clinical trials for cancer, in which cells are engineered to kill themselves if exposed to a certain chemical compound. “If the cell starts to do anything that’s troublesome, you’ll take a pill like doxycycline, and it’ll kill those cells and only those cells,” Melton says.
Teratomas — tumors comprising a variety of tissue types such as hair, bone and teeth — are a particular worry in the use of pluripotent stem cells in therapies, including for regulatory agencies, says stem cell researcher Juan Domínguez-Bendala of the Diabetes Research Institute in the University of Miami Miller School of Medicine. “Nobody can be certain of what may happen when you start transplanting thousands of patients. One single case of a teratoma may set the field back for years.”
And so Domínguez-Bendala, who is developing insulin-producing pancreatic beta cells to treat type I diabetes, has generated human pluripotent stem cells with two kinds of suicide genes. One of them is designed to spring to life in any implanted cell that transforms into something other than a beta cell. The other can be activated in cells that show molecular signs of forming a tumor.
“The immune system is there 24/7, always knocking at the door.”
Lonnie Shea, University of MichiganReporting in the journal Stem Cell Reports in March, Domínguez-Bendala and colleagues found that they could largely prevent tumor formation when the cells were transplanted in mice, and any that slipped through the net could be destroyed. “Our strategy allows us to selectively preserve the cells of interest while killing off everything else,” he says, “and it can be easily adapted to any specific cell.”
Tumors are not the only risk, though. The excitement about universal donor cells is tempered with caution because the immune system has such a full bag of tricks, says Shea, who coauthored an overview of the technology in the Annual Review of Biomedical Engineering. “The immune system is there 24/7, always knocking at the door. If you can do something to protect the cells, that’s a great start, but it has to be on, 24/7 — it can’t weaken.”
It’s unclear, he says, how the immune system as a whole will react if certain cells in the body are chronically making immune-suppressing molecules. Perhaps the universal donor cells initially will engraft and function well, but problems may crop up over time. Maybe the grafted cells will eventually be destroyed. Or what if those cells are infected with a virus — will the immune system be able to eliminate it?
Given such concerns, many immunologists believe that it may be necessary to retrain the immune system — rather than just find ways for cells to dodge its bullets.
Kean’s lab, for example, is looking for a combination of drugs that can be administered for a limited time to reset the immune system so that the transplant is tolerated without interrupting normal protective immunity.
Different types of cells may require different degrees of immune stealthiness, Kean points out. Insulin-producing beta cells ideally will last a lifetime, while heart muscle cells may not need to persist for long if their job is just to offer temporary support while the heart repairs itself.
Adding alternatives
Generating universal donor cells is not the only approach to off-the-shelf regenerative medicine, and this concept may be combined with other therapeutic techniques.
Shea, for instance, works with immunologist Haval Shirwan of the University of Louisville School of Medicine on a method that transplants insulin-producing cells on a microporous scaffold that is coated with molecules designed to blunt T cell attacks. If a short regimen of an immunosuppressant drug is given at the same time, these transplanted cells survive well in lab mice.
Other labs take an even more radical approach — they want to develop drugs that trigger cells in the patient’s own body to reprogram themselves and repair their own tissues. Sana and the biotech startup Oxstem in Oxford, England, are both pursuing this approach.
Overall, researchers say it’s an exciting time in off-the-shelf regenerative medicine — though with plenty of work still to do.
So far, Melton notes, only a handful of functionally mature cells have been created from stem cells, including beta cells, heart muscle cells and certain kinds of skin, retinal and nerve cells. And it’s still years before universal donor cells will be tested in humans.
But he also stresses the potential of the quest. “The promise of this kind of regenerative medicine is not to just find new treatments,” he says, “but to literally find cures for diseases.”




