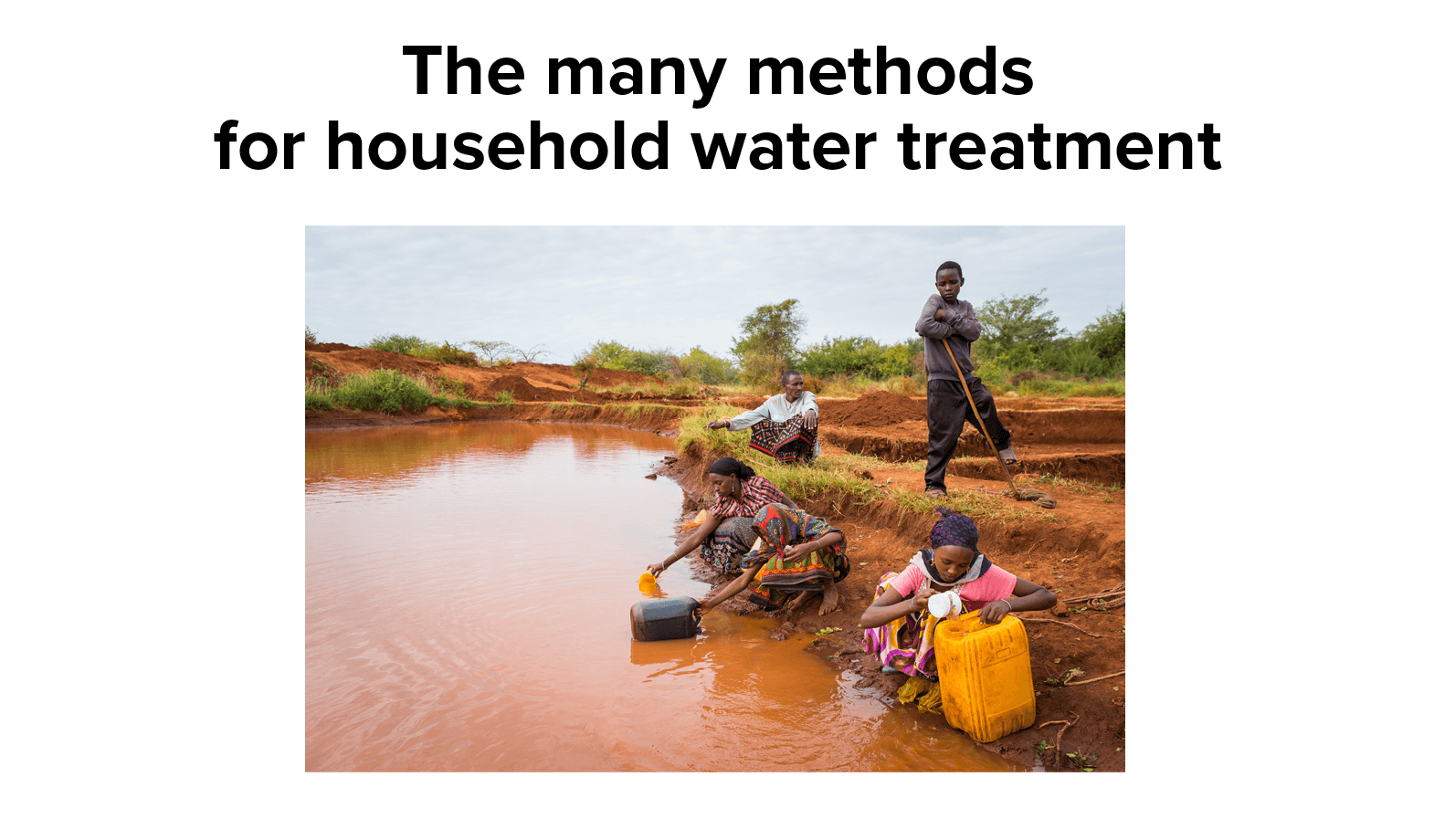
For more than 2 billion people, safe drinking water isn’t a given. Not for them a clean, reliable supply of treated water splurting out on demand from a kitchen tap — instead, they face often long treks to wells, rivers, pools of rainwater or faucets that yield water laced with disease-transmitting feces and other contaminants.
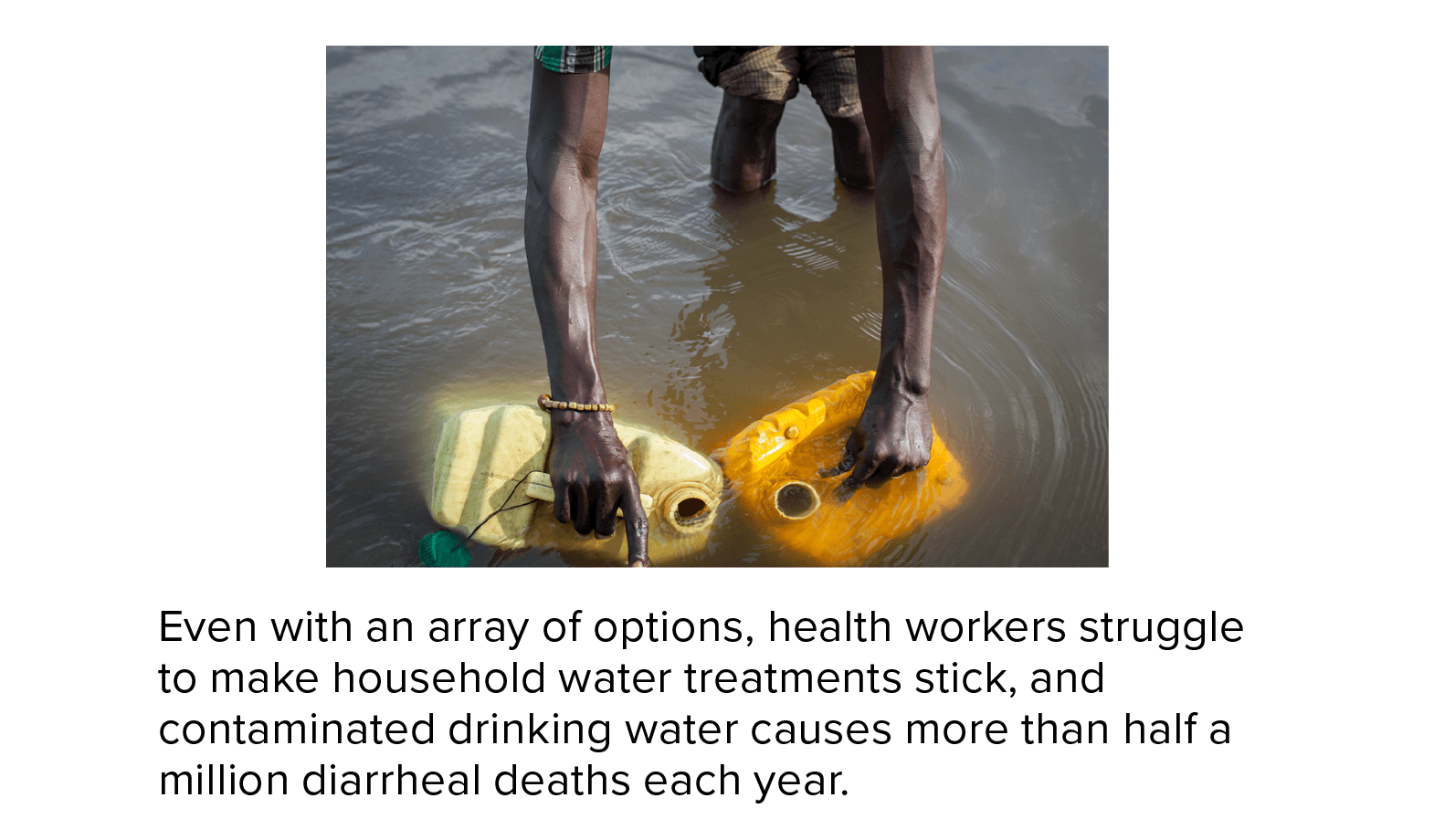
More than 500,000 deaths a year from diarrhea are linked to this very basic lack, and public health officials, philanthropic groups and researchers have worked to move the needle on the problem for decades.
So enthusiasm soared in the early 2000s for a new and compellingly simple approach. Instead of waiting for governments to act, or for projects that progressed at a snail’s pace, what if villages and households were empowered to clean water themselves? A slew of cheap and easy technologies were available for the job.
From Ghana to Afghanistan to Bangladesh, development workers leaped to action. They fitted hand pumps to boreholes in rural communities. They held workshops explaining how a few hours of sunlight could purify water held in plastic bottles. Households received ceramic filters that fit on tables, or larger sand filters cemented outside their doors. Volunteers promoted water-boiling, handed out bottles of chlorine and educated people about threats lurking in even the clearest-looking untreated water.
“Household water treatment was seen as potentially this huge revolutionary new model,” says Joseph Brown, an engineer in public health at Georgia Tech who spent much of his early career designing portable filters. “You could just deliver these devices, and everybody would start using them.”

In some parts of the world, like this community in Indonesia, residents take advantage of the Sun to treat their water. In good weather, six hours of direct sunlight can kill most dangerous microbes in clear water.
CREDIT: SODIS EAWAG / WIKIMEDIA COMMONS
The bad news
Then, in 2009, came the bucket of cold water. A newly published review argued that there was little solid evidence that household water treatment in poor rural regions was working: Placebo-controlled trials in Ghana, Gambia and Brazil found no effect on incidence of diarrhea. Brown recalls that he was giving a talk at the World Bank in Washington, DC, about the benefits of treating water at the household level when, even as he spoke, someone in the audience was circulating copies of the paper.
It was “really the first skeptical paper that had come out around household water treatment — specifically to say that this method for providing safe water is totally bonkers,” Brown says.
More criticism followed. People targeted for interventions didn’t seem to value treatments and weren’t willing to pay for them. They used treatment tools incorrectly or inconsistently, and usage dropped sharply over time. In a trial that taught members of poor communities in Dhaka, Bangladesh, about water safety and supplied 600 households with two free months’ worth of water-treatment products, the devices went largely unused. On site visits, when asked if they had treated their water in the last day, more than 70 percent said no. “Adoption among the global poor is very low,” wrote the study authors, “and little evidence exists on why.”
For public health workers and researchers, it was a huge conundrum. They knew the technologies could make water safe — the methods worked well in laboratory settings — so what was stopping these simple solutions from taking hold in the real world, with the people who needed them most? That puzzle has spurred a sea change in research around water development. Where once investigators asked what tools were best to gift to communities, they now ask why those “gifts” may have no impact. Questions of engineering and chemistry have given way to quite different questions about policy, maintenance — and the realities of human behavior.
“There’s no technology that eliminates the need for implementing well,” says Millie Adam, director of international partnerships at the Canadian charity Centre for Affordable Water and Sanitation Technology (CAWST). “There’s many organizations that have tried to find the silver bullet that you can just drop in, do it, and then check that community off the list and walk away. I don’t think that solution exists.”
From lab to field
In 2015, member states of the United Nations set a package of development goals including universal safe water by the end of the next decade, with the ideal being safe, piped water delivered to homes and communities. The world is nowhere near on track. Most researchers, public health officials and development workers agree that household water treatment options can be crucial as interim solutions in emergencies or where no other resources are available — but experts are still divided on the role household water treatment should play in filling the gaps long-term.
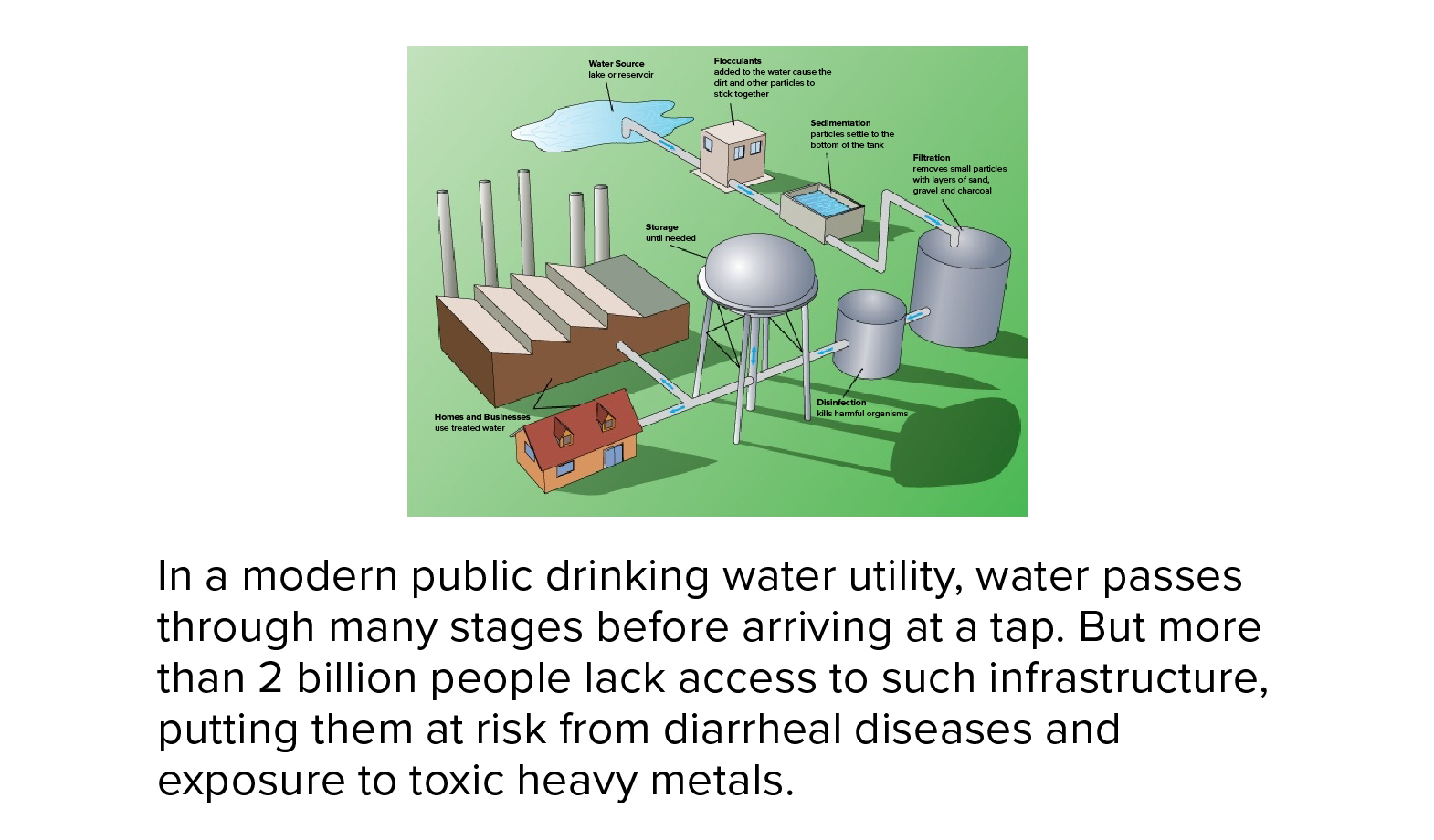
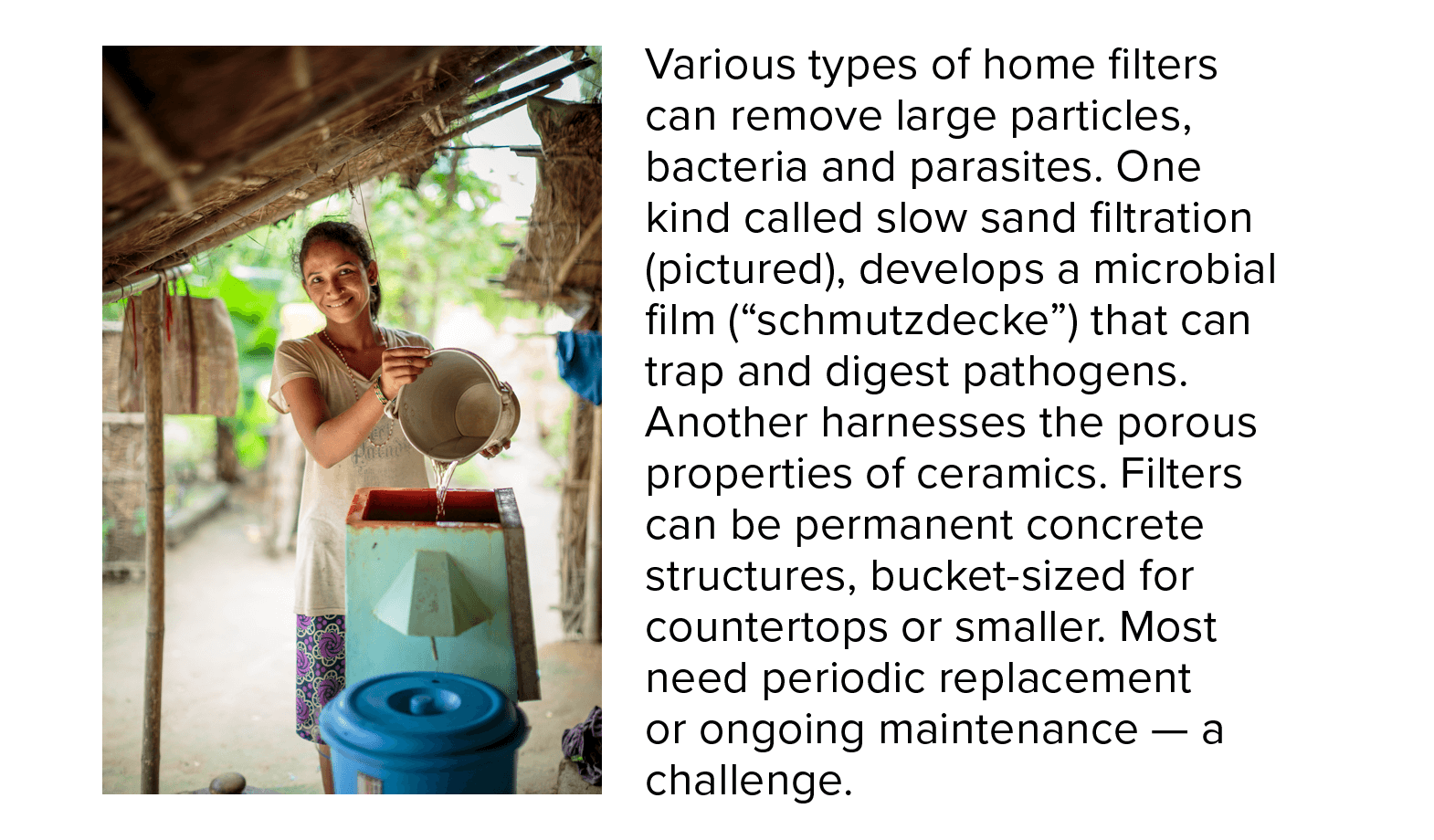
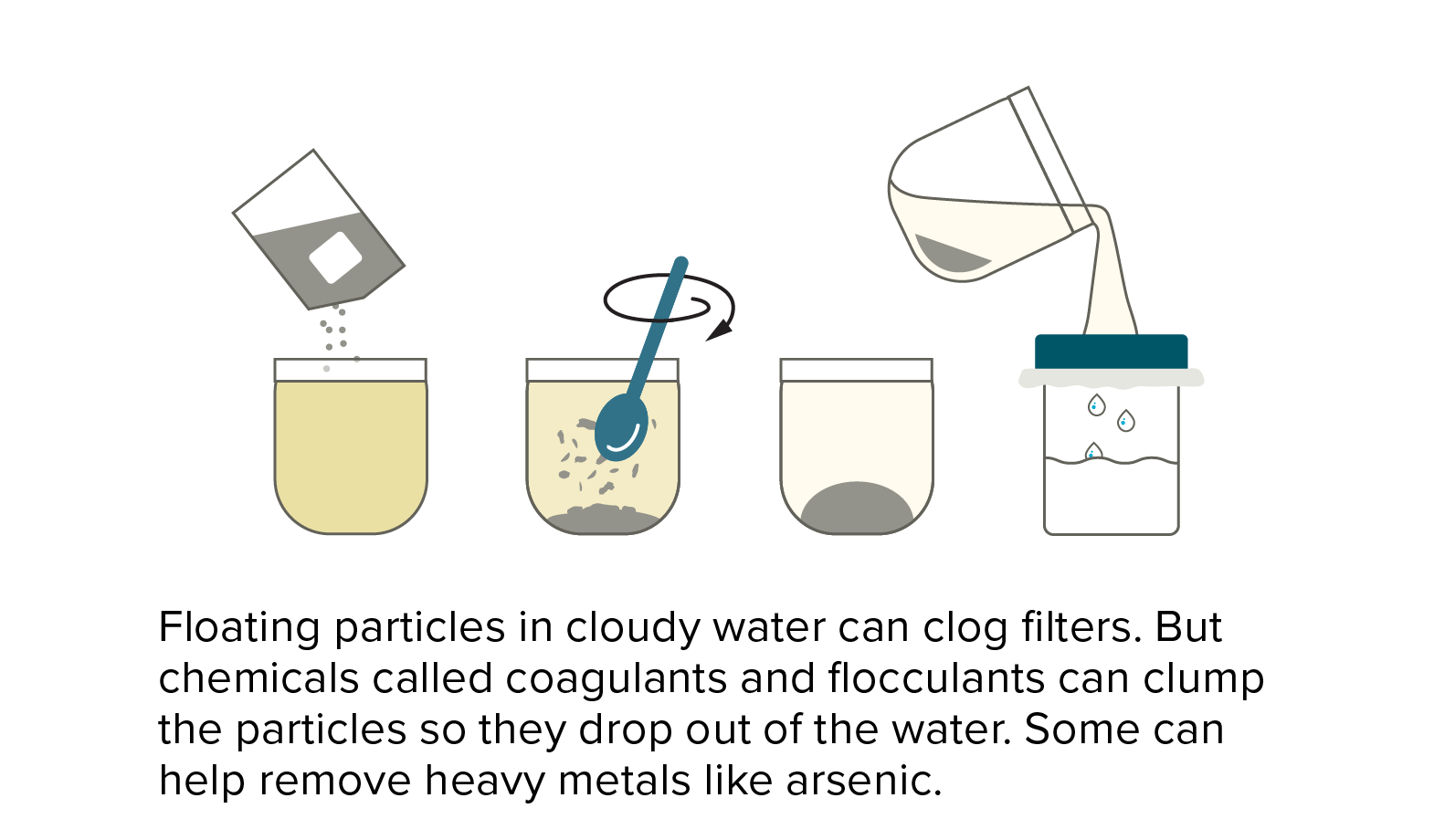
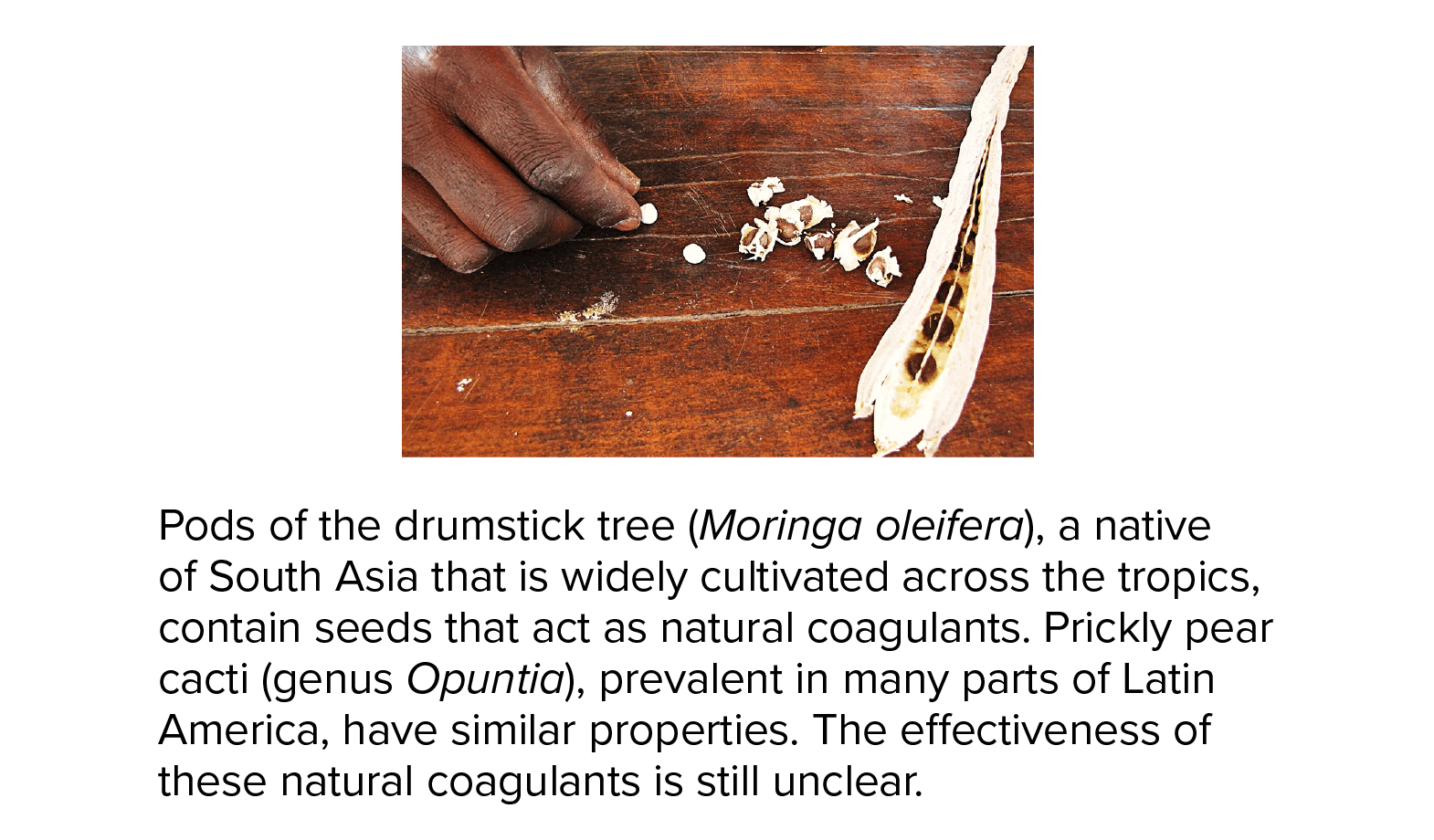
An abundance of cheap solutions can mimic the process that water goes through at a modern large-scale municipal utility. Chlorination, filtering and disinfection by heating water in the sun can kill or remove more than 90 percent of microbial pathogens in laboratory settings, while boiling, when done properly, kills 100 percent of the microbes causing diarrheal diseases.
But lab success doesn’t necessarily translate to field victory, and there are many reasons why.
Durability is one of them. A 2009 study that evaluated use of ceramic filters in 13 villages in rural Cambodia found that filter use declined at a rate of 2 percent each month, due mostly to breakage of spigots, containers and ceramic filter elements. Four years out, filtering had practically ceased. And a 2016 study of ceramic candle filters in a village in South Africa found that the filters stopped working properly months earlier than expected due to higher-than-expected levels of use. Eight months after distribution, people were still using the filters, but none produced water free from contamination.
A lack of long-term planning and follow-up has left behind a legacy of failure. As noted in a March 2009 briefing of the International Institute for Environment and Development, an estimated 50,000 African boreholes and wells, dug to tap safe sources of groundwater, were no longer working due to lack of plans for basic upkeep. “Rather than construct a thousand wells, I’d rather construct 800 wells and put aside a chunk of money for maintenance,” says Michael Kremer, a developmental economist at Harvard University.
Purification, with imperfections
Long-term planning matters even for the simplest modes of water treatment. Boiling, the most common purification method, is used by around 20 percent of households in low- and middle-income countries. But not all boiling is equal. Whereas electric boilers can be safe and efficient, using other forms of fuel can be costly and even dangerous. Collection or purchase of fuel is a burden, and household air pollution from burning solid fuels such as wood, charcoal and animal dung causes more than 3.5 million premature deaths annually.
Chlorine is favored as one of the cheapest options for water treatment — 1,000 liters of water can be treated at a cost of only 10 cents.But households without taps must store water for extended periods, so chlorine levels must be high to protect against recontamination, imbuing water with an acrid smell and taste. Chlorine is also less effective in cloudy or muddy water. And even though it’s cheap, users must still mix the appropriate amount with the water and wait for the chemical to take effect.

Indoor air pollution from traditional stoves that use solid fuels, such as wood, charcoal or animal dung, can spark health consequences ranging from pneumonia to heart disease. For the approximately 3 billion people who still use solid fuels to cook, the need to boil water means more dangerous exposure time. In this photograph, a young girl in Tanzania is tending an indoor cookstove.
CREDIT: AURORA PHOTOS / ALAMY STOCK PHOTO
In circumstances where people are poor and already overworked, these small extra steps can doom a process that needs to be done right to work, says Isha Ray, an economist specializing in water and development at the University of California in Berkeley, where she co-heads the Berkeley Water Center. Ray doubts that she herself would do much better if she were in the same position. In fact, she says, research suggests she wouldn’t.
“One thing we know from the social sciences is people are not all the time driven only and exclusively by health considerations,” she says. “Every single person I know has a gym membership they don’t use, including myself.” How then, she asks, is it practical to expect a person with fewer resources and more daily chores to take on the additional burden of treating water? Lugging and treating water can be a “painful chore that has to be repeated every day,” she says, one that typically falls to women. “And that means her body is acting as infrastructure, covering for a piece of pipe.”
And anything short of perfection may reap few returns, according to a 2012 modeling study coauthored by Brown. It found that skipping treatment of high-risk water just 10 percent of the time would result in a 96 percent drop in the potential health benefits.
Keeping it simple
So it would make sense that the most effective approach would be to make water treatment as automatic as possible, eliminating extra steps. Behavioral research is starting to confirm this.
In a study in Kenya that ran from 2007 to 2011, chlorine dispensers were placed right next to pipes providing continuous water flow where villagers went daily to fill up their jugs. After filling a container, all the villager had to do was place it under a chlorine dispenser and turn a knob. The walk home took care of mixing. That convenience seemed to pay off: Three and a half years later, 51 percent of village participants had adequate levels of chlorine in their water, compared with only 6 percent of people in similar villages. Those people received only promotional messaging about the value of chlorine, then had to go pick it up themselves.
Kremer, who worked on the project, says he’s excited about efforts to go one step further and design completely automatic chlorine dispensers that apply the right amount of chlorine as water is collected at taps. Removing extra steps also applies to payments, he says: People will pay for access to water, but often not the cleanliness of water. Thus, bundling the costs together should be more effective than adding a separate fee on top.

A girl in Kenya chlorinates her water. Chlorine dispensers placed next to water collection points save time and effort for people who already must make long treks to get water. Mixing happens automatically during the walk back.
CREDIT: THOMAS CHUPEIN FOR J-PAL
The right kind of information may be powerful, too. In a 2018 study, researchers gave poor families in rural India water-safety education and the means to get readings on water quality in their own households, either through self-administered test kits or laboratory reports. After a month, participants who received such information reported boiling their water more consistently than participants who just received water safety education, and their water also had a bigger drop in E. coli levels.
Brown, one of the lead authors, thinks direct feedback like this might help people get involved in tackling their water issues. “Most water that’s unsafe looks and smells perfectly fine. The challenge is making this invisible problem visible,” he says.
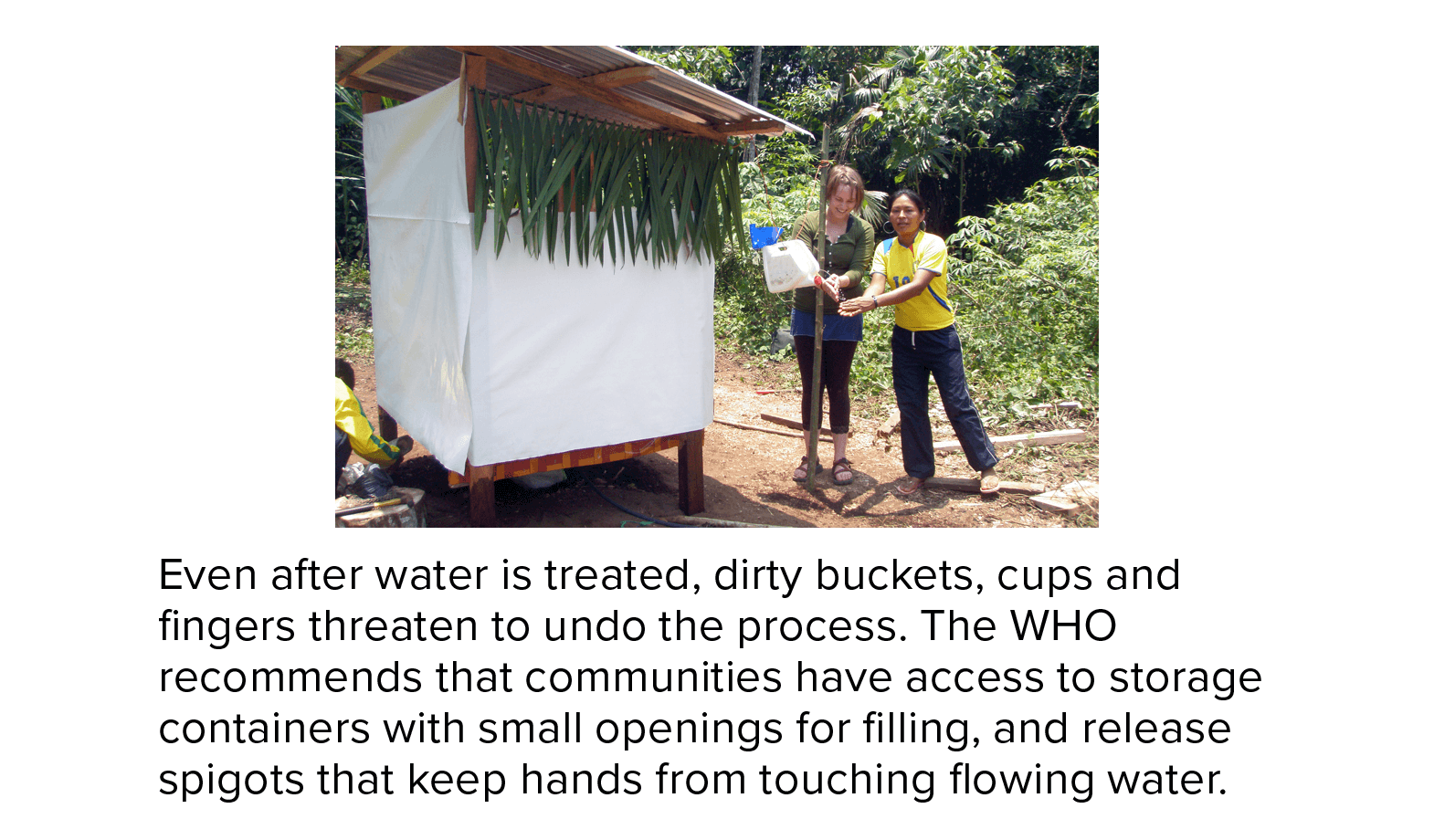
Dry facts, but no easy answers
Researchers are investigating a number of other factors they suspect might improve water treatment efforts. Some studies, with mixed results, have examined whether establishing leadership roles for women — who are often responsible for a household’s water supply — could improve long-term adherence to water treatment. And researchers who worry that offering free water treatment might undervalue the service in participants’ eyes have suggested that vouchers for chlorine and other treatments might help convey that value without precluding treatment for those who can’t pay. Other questions linger around how to effectively educate people on safe water storage and use: Often, community leaders are more persuasive than foreign development workers, and the nuances of marketing can be crucial.
The solution for one community may well be unsuitable for another. Romain Villiers, global water, sanitation and hygiene advisor for CAWST, spends months learning about a community before recommending a water treatment project. Sometimes, two settings can feel “like working on different planets,” he says, making it daunting to predict what will work. Even gold-standard controlled trials — ones comparing people who received an intervention to ones who didn’t — won’t tell you if results will generalize to other communities.
For that reason, some global health researchers are experimenting with statistical analyses across interventions in different communities. By assigning scores to factors such as financial management and community cooperation and comparing them across interventions, they hope to tease out common drivers of success.
A 2014 study used such a method to evaluate sanitation and hygiene programs across 16 schools in rural Bangladesh. The study found that schools continuing to have working toilets usually had higher financial contributions from local governments or communities than schools where toilets ended up broken, unclean and unusable. In the rarer cases where toilets remained functional without higher financial support, schools had concrete maintenance plans and a “local champion” — typically a teacher or project field officer — who oversaw regular cleaning and maintenance.
In a similar vein, a 2018 study sought to identify common features of successful drinking water systems by analyzing shared characteristics of 20 cases across the globe. Though the researchers couldn’t consider all the factors they were interested in, they did identify good financial management and community involvement in project decisions as two critical ingredients.
The importance of those two factors makes ample sense to Christie Chatterley, an environmental engineer at Fort Lewis College in Colorado who worked on the Bangladesh sanitation study and spent her early career working on sanitation, water and energy projects for low- and middle-income countries. One of them was a community water-treatment system in Rwanda that combined a settling tank, sand-based filtration and solar-powered ultraviolet disinfection.
“In the US you have a municipal system, and there are all sorts of regulatory bodies.... We forget that we rely on these systems, and we go into low-income countries and we think the infrastructure is going to be enough.”
Christie ChatterleyThat technology should have worked, she says: “Everyone thought, ‘It has to — it’s designed so perfectly!’” Except it didn’t. Missing from the plan was adequate attention to less sexy but critical questions of long-term maintenance, monitoring and funding.
“In the US you have a municipal system, and there are all sorts of regulatory bodies, and we have water meters, and we have people checking on things and making sure the treatment is adequate,” Chatterley says. “We forget that we rely on these systems, and we go into low-income countries and we think the infrastructure is going to be enough.”
These days, Chatterley focuses on water policy and “systems building” — industry-speak for helping communities establish the support, planning and resources they need to keep a project going. It may not be a glitzy term but there is no getting around it, she says. It’s why the projects that are likely to last take so long to set up.
Creating water-wise policies, supply chains, financial management, monitoring systems and all the other pieces needed to keep a project going is slow work. But building these systems may be the most important part of meeting the United Nations goal of getting safe water to everyone in just over a decade, researchers say.
“You would think with all the resources and knowledge in the world, we would be able to figure it out by 2030,” Chatterley says. “But when you look at the reality of things, then it does feel really daunting.”