When my grandmother Carol Mitchell was diagnosed with Parkinson’s disease in 2010 at the age of 72, she was prescribed a drug called carbidopa/levodopa. She swallowed the little oblong pill four times a day — 7 a.m., 11 a.m., 3 p.m. and 7 p.m.
In the years that followed, her doctors prescribed her a steroid cream for skin issues and drugs for depression, motion sickness, anxiety, acid reflux and early breast cancer. “I walked into her bedroom and there were vials everywhere,” says Elizabeth Mitchell, Carol’s daughter and my mother. “I was Googling each one to see what they were for.”
For Carol, who is now 82, taking all her drugs precisely when she’s meant to has been a tough goal. “I don’t want to take medications like that. It’s too much, I think,” she says. “You can’t leave the house because you’ve got all these medications to take.” Inevitably, she would find herself missing doses of her Parkinson’s drug — and when she did, her symptoms of tremors, stiffness and difficulty with speaking and walking would return or worsen. In the last four years, that has led to four emergency department visits, two of which involved extended hospital stays.
To make taking the essential Parkinson’s pill easier, Elizabeth suggested that her mom wean herself off as many meds as she could with her doctor’s help, and today, Mitchell takes only the Parkinson’s drug. “I feel much better being on less medicines,” she says. Elizabeth says that her mom is far more likely to take her carbidopa/levodopa at the correct time now, helping to keep her out of the hospital.
But for many other elderly patients who are on multiple medications, weaning is not so easy.
Polypharmacy, often defined as the regular use of five or more drugs by one patient, is on the rise and is expected to grow as life expectancy increases and the global population ages. Elderly people not only take more drugs but also face a greater risk of severe side effects because their livers tend to be less efficient at metabolizing and clearing medications from the bloodstream. This risk is exacerbated by the fact that interactions between some drugs can be harmful and up to half of patients taking four or more drugs do not take them as prescribed, according to a 2020 analysis in the Annual Review of Pharmacology and Toxicology.
The US population is graying. In step with that trend, the problem of polypharmacy is predicted to grow.
The World Health Organization considers polypharmacy a major public health issue, contributing to the millions of hospitalizations that occur globally due to adverse reactions to drugs and responsible for billions of dollars in unnecessary health expenses. Researchers and pharmacists are grappling with how to solve this overmedication problem.
But doing so is difficult, not least because deprescribing, or stopping, a patient’s medications is rarely taught when drugs are covered in medical or pharmacy school. “There’s not even the discussion that you need to check whether the balance of harms and benefits is constant over time,” says Tobias Dreischulte, a clinical pharmacist at Ludwig Maximilian University in Germany and one of the authors of the Annual Review paper.
But it’s doable, adds Dreischulte. He earlier did research at the University of Dundee in Scotland and is part of a team that published a series of guidelines to help that country’s doctors and pharmacists reduce the use of unnecessary or potentially dangerous medications. Since the guidelines’ implementation in 2012, the number of excess medications and high-risk drug combinations prescribed to patients has dropped.
The question is whether similar practices can be applied to other countries throughout the European Union and across the globe. “Historically, clinical treatment guidelines don’t have any recommendations or comment on how or when to stop medications,” says Emily Reeve, a researcher and pharmacist at the University of South Australia in Adelaide, who has been studying ways to reduce the impact of polypharmacy in older adults for the past decade. “How can we make deprescribing a part of regular practice?”
A drug-obsessed health care system
Worldwide, the number of adults age 65 and up is on the rise. In the United Kingdom, for example, the number of older individuals is projected to increase by 67 percent — or an additional 8.2 million people, a population roughly the size of modern-day London — from 2019 to 2068. In the United States, the portion of older adults is expected to rise by about 81 percent, or 42.3 million more people, from 2018 to 2060.
As people age, chronic medical conditions, from osteoporosis to cardiovascular disease to cancer, become more common. And for medical systems across many countries, prescribing drugs is the go-to method to treat these illnesses. According to a report by the Lown Institute, a nonprofit think tank, 42 percent of all older adults in the US take five or more prescription medications a day. Almost 20 percent take 10 drugs or more, and over the past 20 years, incidences of polypharmacy have tripled across the country.
This chart shows how polypharmacy is growing among older adults in the US. It comes from a 2019 report by the Lown Institute, a nonpartisan think tank, on the extent of the polypharmacy problem. “Over the past few decades, medication use in the US, especially for older people, has gone far beyond necessary polypharmacy, to the point where millions are overloaded with too many prescriptions and are experiencing significant harm as a result,” the report states.
The pharmaceutical industry’s for-profit model may influence doctors to prescribe more medications, according to an investigation by the newsroom ProPublica. They reported that doctors who receive money for a specific drug prescribe that drug more often than doctors who aren’t benefiting financially. In 2015, about half of all doctors in the US accepted payments from drug companies, totaling $2.4 billion.
Another contributing factor is the disconnect between a patient’s different doctors, leading to prescribing without proper communication. Consequently, what seems to be a novel illness may in fact be the side effect of a drug. “All the specialty doctors just focus on their area,” says Grace Lu-Yao, a cancer epidemiologist at Thomas Jefferson University in Philadelphia. Many patients, including those with cancer that Lu-Yao studies, don’t have a doctor who can help them see the overall picture of their treatment and health. “Who,” she asks, “will be the person to look out for potential interactions, or to stop some medication?”
Sometimes, of course, it’s necessary to prescribe multiple drugs at once. For example, to stop a patient who’s had a heart attack from having another one, treatment can include medications that lower cholesterol, reduce blood pressure and stop blood cells from sticking together.
But when the risk of the medications outweighs their potential benefits, patients are in danger of significant health consequences. Every day, 750 older adults are hospitalized due to serious side effects from their medications, including falls, allergic reactions and internal bleeding. And with each additional medication prescribed, the risk of an adverse reaction increases by 7 to 10 percent.
The whole system is set up improperly, says Lu-Yao. In a study published last March, she and her colleagues examined hospitalization rates of prostate, lung and breast cancer patients following chemotherapy treatment. Compared to patients taking fewer than five medications, prostate cancer patients taking five to nine, 10 to 14, and over 15 drugs had respectively 42 percent, 75 percent, and 114 percent higher rates of hospitalization after chemotherapy. Patients with breast and lung cancer had similar patterns. (The group taking more drugs did not appear to have been sicker than those taking fewer drugs, based on hospitalization rates in the six months before the chemo treatment.)
If trends continue, it’s estimated that polypharmacy will lead to nearly 150,000 premature deaths in the US over the next decade, according to the report by the Lown Institute. It will also be responsible for at least 4.6 million hospitalizations in the US between 2020 and 2030, costing around $62 billion, the report predicted.
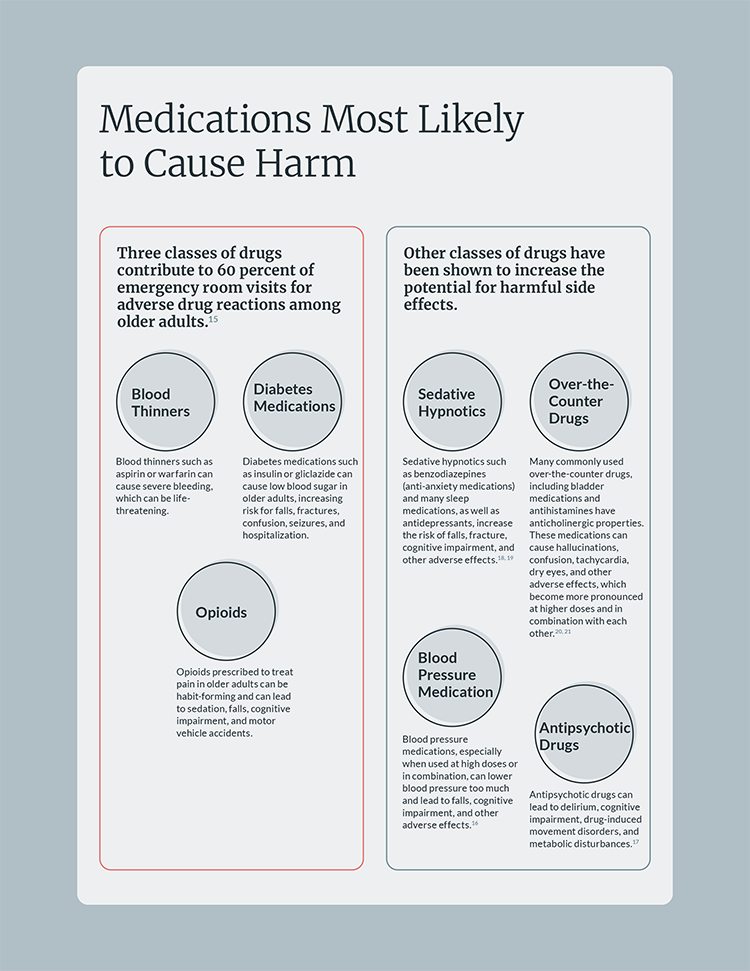
Certain drugs are especially risky for older adults and warrant care in prescribing and monitoring, experts say. Here, from a report by the Lown Institute, is a cheat sheet of the classes of drugs that are most likely to cause problems.
CREDIT: LOWN INSTITUTE, WWW.LOWNINSTITUTE.ORG
Deprescribing made easier
Pushing for a health care system that promotes more judicious drug use and deprescription is extremely difficult, Reeve says. But patients seem open to trying: In 2018, a nationally representative survey by Reeve and her colleagues suggested that 92 percent of older adults in the US are willing to stop taking one or more of their medications if their doctor says it’s possible. But many doctors lack the educational resources to do so safely. There are some general and drug-specific deprescription guidelines, along with websites such as the electronic deprescribing tool MedSafer that guide doctors and pharmacists through the process — but few of these have been shown to work in clinical practice.
“Deprescribing itself is not a simple action,” says Reeve, who is working to create deprescription guidelines that could be used internationally. “It’s not something that can happen within a 10- or a 15-minute appointment.” It involves identification of a potentially unnecessary or dangerous drug, an agreement between doctor and patient to deprescribe the drug, and often a slow tapering of the medication while the patient is closely monitored.
Scotland’s polypharmacy guidelines by drug and health care experts, first published in 2012, were designed to fill this resource gap and aid clinicians throughout the prescription and deprescription process. The effort’s “7-Steps” technique encourages doctors to carefully review a patient’s diagnoses and treatments, determine which drugs the individual needs, identify potential adverse drug reactions and ensure that the patient is involved in the decision-making process.
An evaluation of the guidelines reported that from 2012 to 2018, there was a notable reduction in the number of high-risk drug combinations prescribed to older adults, according to data collected by Scotland’s health care system. This included a particularly dangerous combination: use of nonsteroidal anti-inflammatory drugs like aspirin; high-blood-pressure medications such as angiotensin II-receptor blockers that relax the veins and arteries; and diuretics, which help to rid the body of excess salt and water through urine. Known as the “triple whammy,” this amalgamation can lead to kidney and heart failure — especially in older patients with a history of liver disease.
More broadly, use of these guidelines over the six-year period resulted in the deprescription of more than 120,000 inappropriate medications annually.
After a succession of deprescribing guidelines were published in Scotland in 2012, 2015 and 2018, prescription rates fell for a risky drug combination known as the “triple whammy”: nonsteroidal anti-inflammatories in combination with diuretics and ACE inhibitors/angiotensin II-receptor blockers. The vertical axis (“PRM14”) shows the percentage of Scottish patients aged 65+ who were prescribed the risky combination. PG1, PG2 and PG3 are the dates when the three guideline editions were published.
Changing the culture
Now it’s a matter of whether health care systems in other countries can implement similar guidelines. “It is entirely possible, but it will take time,” Dreischulte says. He thinks that these changes will be easier to make in countries with centralized medical systems such as the UK, where the National Health Service, or NHS, is publicly funded and the government runs hospitals and employs doctors. As a result, the NHS “is very effective in getting evidence-based medicine across to practicing clinicians,” he says.
Health care in the US, on the other hand, is highly splintered. As of 2019, 68.5 percent of the US population was covered by private health insurance, almost 43 percent had public coverage such as Medicare and Medicaid, and just over 9 percent were uninsured. (Some individuals have more than one type of coverage at a time.)
Still, some US strides to address polypharmacy are underway. One is the Age-Friendly Health Systems program, developed in 2017, in which hospitals and medical care settings agree to adhere by the 4Ms — a set of guidelines that ensures reliable care for the elderly by prioritizing what matters in their lives, along with their medication, mobility and mentation, or cognitive abilities. The medication element involves health care professionals asking if a drug is necessary for the patient, avoiding prescription of high-risk medications, establishing a plan for safe dose adjustments and deprescribing when needed.
By the end of 2020, more than 1,950 health care organizations nationwide had joined the Age-Friendly Health Systems initiative. Those that implemented the 4Ms reported reduced numbers of hospital readmissions, deaths and cases of delirium. They also reported cuts in health care costs. The goal is to reach a total of 2,600 organizations by June 2023.
This chart, of data from Scotland, shows how polypharmacy increases with age as medical problems (such as cardiovascular disease, diabetes and arthritis) pile up for a person. It also shows that the degree of deprivation — a measure encompassing things like income, housing, education and access to services — has an effect as well. Displayed for each age group are five bars that indicate the highest to lowest levels of deprivation (quintiles). In every age group shown, polypharmacy rates are higher for groups that are more deprived. (SIMD = Scottish Index of Multiple Deprivation. SAPE = small area patient estimate.)
It’s also possible that some large US health care systems with more joined-up patient care could implement deprescription strategies. Justin Turner, a researcher at the University of Montreal, points as an example to a study of community pharmacies in the Montreal area: It showed that giving elderly patients who regularly take benzodiazepines like Valium and Xanax — some of the most overprescribed medications — a brochure about the benefits and harms of these drugs is an effective way to stop drug overuse. Of patients who received the brochure, 27 percent stopped taking their benzodiazepines within a six-month period, compared to only 5 percent of those who did not.
Pharmacies that are linked by a health care system in the US could potentially do likewise, Turner adds. He is collaborating with researchers at the University of Washington who are leading a trial with the nonprofit health system Kaiser Permanente in that state; its aim is to reduce falls among older adults through deprescribing unnecessary, high-risk drugs. Turner is also collaborating with researchers at the Philadelphia VA Medical Center on another project aimed at education and reduced use of risky medications.
Studies like this may become more common in the US. In 2019, the US Deprescribing Research Network, a community of pharmacists, clinicians and scientists, was established. The group is funded by the National Institute on Aging and offers resources like pilot grants to those who are developing and disseminating research on deprescription in older adults. “I think the tide is changing,” Turner says.
In the meantime, many elderly patients who are already on multiple drugs have the extra burden of being their own advocates. Or they must depend on family members and loved ones to push for deprescription when necessary.
Just this February, my grandmother visited her doctor and was prescribed the amphetamine Adderall to help with her daytime drowsiness, a symptom likely caused by the carbidopa/levodopa she must take for her Parkinson’s. Alarmed, her daughter Elizabeth contacted Carol’s doctor. “I cannot stress enough that new pills are not the answer for Mom’s case,” she wrote in a letter. Instead, “she needs a caregiver, she needs exercise, she needs social interaction such as Zoom calls with her church group.”
The doctor responded quickly, and Carol is not taking Adderall, and that’s how Elizabeth would like it to stay. She does what she can to help her mom take her Parkinson’s drugs on time — even that single medicine remains a challenge — and sees a huge change at the times when the regimen is followed and her mom also takes regular two-mile walks.
“She is at her bandwidth on just dealing with one medicine four times a day. She can’t handle any more additions to that,” Elizabeth Mitchell says. “When she adds to that, she misses the carbidopa/levodopa and just ends up back in the hospital.”




