Say you’re feeling depressed, distressed, helpless or anxious. Whom should you turn to for professional help? A cognitive behavioral therapist, who’d challenge your dysfunctional thoughts? An old-fashioned Freudian analyst, who might have you lie on a couch, spending months, maybe years, and thousands of dollars delving into your unconscious responses to the ways your parents raised you? But what if all you need is a much less expensive social worker — or even a life coach?
These questions have fueled a fierce debate among researchers and clinical practitioners. The argument isn’t whether “talk therapy” is helpful. Hundreds of clinical trials have shown that various mainstream forms of psychotherapy can help treat many mental afflictions, including depression, anxiety, post-traumatic stress, obsessive-compulsive disorder and eating disorders. Indeed, most Americans prefer talk therapy to medication, and talk therapy alone may work just as well and in some cases last longer than medication for some mental health problems. The argument is more about how and why these treatments work, and, accordingly, which therapeutic approaches are most likely to achieve the best results at the lowest cost.
On one side are those who say choosing the right approach is essential, implying that some strategies are clearly better than others. The other side argues that any good therapist will do, because factors common to most psychotherapies — especially a strong bond between patient and therapist — are what’s most important. In between these two camps, but just as involved in the debate, are agnostics who argue that it’s too soon to choose sides — we still just don’t know enough about how therapy works.
There are high stakes in this dispute. “This isn’t just about a bunch of academics fighting each other,” says Bruce Wampold, a psychologist now retired from the University of Wisconsin–Madison. “There are tremendous implications for how mental health care is delivered and managed.” More and more mental health patients are being treated solely with medication prescribed by general practitioners, with many talk therapists voicing concern that insurance firms and health plans are threatening their profession in their efforts to cut costs. And even when patients are given access to talk therapy, insurers tend to push for the cheapest, most time-limited strategies, which are often “not in the interest of patients,” Wampold says.
Antidepressants have replaced psychotherapy as the main treatment for depression in the United States. Use of psychotherapy continues to decline.
The dodo bird verdict
People have been trying to talk other people into feeling better for more than 3,000 years. Ancient Greeks counseled patients suffering from addictions and psychoses. For nearly 2,500 years, Buddhists have handed down a canon of advice to people struggling with day-to-day emotional suffering. But it was only at the end of the nineteenth century that the Austrian neurologist Sigmund Freud popularized the “talking cure.”
These days, more than 130,000 licensed US psychiatrists and psychologists provide what is often a blend of Freudian-ish psychodynamic therapy (focused on childhood experiences) and cognitive behavioral therapy (focused on challenging negative thought patterns). But you can also receive some version of talk therapy from a social worker, counselor or marriage and family therapist — or conceivably even from a life coach, mentor, hypnotist, neurofeedback practitioner or shaman (see sidebar below).
In 1936, the eminent US psychologist Saul Rosenzweig proposed that a therapist’s preferred method was all but irrelevant. Instead, he wrote, factors common to most therapies will determine the outcome more strongly than any of the therapy’s specific features.
“Given a therapist who has an effective personality and who consistently adheres in his treatment to a system of concepts which he has mastered and which is in one significant way or another adapted to the problems of the sick personality, then it is of comparatively little consequence what particular method that therapist uses,” he wrote.
Rosenzweig began his iconic paper with a passage from Lewis Carroll’s Alice’s Adventures in Wonderland in which a dodo bird, judging contestants in a race, declares that all have won “and all must have prizes.” He thus set the stage for the long-running debate over what has since been known as the dodo bird verdict.
“All must have prizes,” the dodo told Alice after a race in Wonderland. Are all psychotherapy methods also winners? An influential twentieth century scholar proposed the idea.
CREDIT: BRYAN SATALINO
In subsequent years, researchers identified several potential “common factors,” ranging from the therapist’s office environment to the placebo effect, which has a strong role in both talk therapy and medication. Yet at the top of the list of factors is the relationship, what’s called the therapeutic alliance, between patient and therapist.
The reasoning is that this positive emotional bond, made up of trust, respect, affection and high expectations for improvement, inspires each member of the pair to keep showing up and doing the hard work that therapy demands. Specifically, researchers have found, a strong alliance will help the therapist and patient reach consensus on their goals, as well as on what sort of tasks — such as free association, Socratic questioning, or homework — will help achieve them.
Sixty years after Rosenzweig put his stake in the ground, Wampold and colleagues reviewed more than 200 scientific studies comparing the effectiveness of mainstream therapies, mostly variants of psychodynamic and cognitive-therapy tactics used by well-trained practitioners. They found only minimal differences between outcomes, concluding that “bona fide treatments are roughly equivalent.” (That conclusion may not extend to outlier therapies such as shamanism, Wampold and other researchers warn, which haven’t been sufficiently evaluated.)
The bottom line, according to Wampold, is: “You can’t have psychotherapy without a relationship. Every patient knows that. And every psychotherapist knows it.”
The bond between therapist and patient has a bigger impact on the success of psychotherapy than the type of therapy, studies find. “Other factors” include everything that happens outside the therapist’s office, including other events in the patient’s life and society as a whole.
In recent decades, researchers have published scores of papers emphasizing the importance of the bond between patient and therapist. In 2018, a task force for the American Psychological Association concluded: “The psychotherapy relationship makes substantial and consistent contributions to outcome independent of the type of treatment.”
In 2019, however, psychologist Pim Cuijpers, a leading agnostic, weighed in with a paper in the Annual Review of Clinical Psychology arguing that we’re still far from knowing how talk therapy works.
Earlier studies have been inconclusive, wrote Cuijpers and two colleagues at Vrije University Amsterdam. They cited flaws including researcher bias in favor of particular therapies and an excess of papers that show an association between a treatment and an outcome without proving which facet of the treatment caused the outcome. What’s more, they suggested, some studies purporting to compare different therapy types tip the scales by comparing the researchers’ favorite with another form of therapy “designed to fail” — in other words not a tested, bona fide strategy.
Solving the mystery once and for all will require much more work, they wrote, adding: “It is as if we have been in a pilot phase of research for five decades.”
In a 2007 review, Yale psychologist and child psychiatry researcher Alan Kazdin voiced a similar complaint, urging researchers to focus their studies on the ways that the patient-therapist relationship may be helpful rather than simply determining that it helps. “How does one get from ‘my therapist and I are bonding’ to ‘my marriage, anxiety, and tics are better’?” Kazdin asked in his paper. “This is a leap with the intervening steps unspecified or untested, at least to my knowledge.” Reached by Knowable, Kazdin said that after 13 years, he still sees this gap in the research.
In recent years, some professional organizations have vouched for some psychotherapies over others, based on a preponderance of evidence that certain methods lead to good outcomes for specific diagnoses. The treatments most often touted as having strong research support have been versions of cognitive behavioral therapy (CBT), which one organization, the Society of Clinical Psychology, recommends for everything from adult attention-deficit hyperactivity disorder to obsessive-compulsive disorder to irritable bowel syndrome.
Critics note, however, that CBT’s clear rules and comparatively brief time frames have made it easier to study experimentally than more complex, open-ended therapies, thus yielding more net evidence that it gets results without proving that it is better or worse than any other therapy. Indeed, in recent years, some experts have challenged CBT’s reputation as the “gold standard,” with research suggesting that longer-term, psychoanalytic therapy can be more effective in some cases.
Wampold argues that a greater diversity of options will allow therapists and patients to find the approach that works best for them. “Unless there’s convincing evidence that one treatment is superior,” he says, “you should allow therapists to give the treatment they can deliver most effectively and patients should have the right to choose the treatments they prefer.”
Patient preferences do make a difference. In a 2018 meta-analysis of 53 studies involving more than 16,000 patients, researchers called such preferences “crucial” to outcomes. The authors advised that psychotherapists should educate patients about different types of talk therapy and elicit their preferences as to the therapists’ strategies.
Bring in the scans
Any resolution to this long-running conflict may ultimately come from the lab, and its so-far elusive promise of delivering indisputable biological evidence of the most effective treatments.
Some researchers are now using functional magnetic resonance imaging scans to track subtle changes in certain brain regions during and after psychotherapy. One day, perhaps, therapists will be able to post before-and-after scans of patients’ brains, highlighting the improvements, much as plastic surgeons do today. But not yet. The studies so far have mainly focused on laying the groundwork by determining which areas of the brain are affected by therapy, says University of Pittsburgh psychiatrist Jay Fournier. Researchers want to pinpoint how the brain changes in each patient as a result of different treatments and what sorts of changes best predict long-term recovery. They also hope to gain a more nuanced understanding of which characteristics in a patient might predict response to different sorts of treatments.
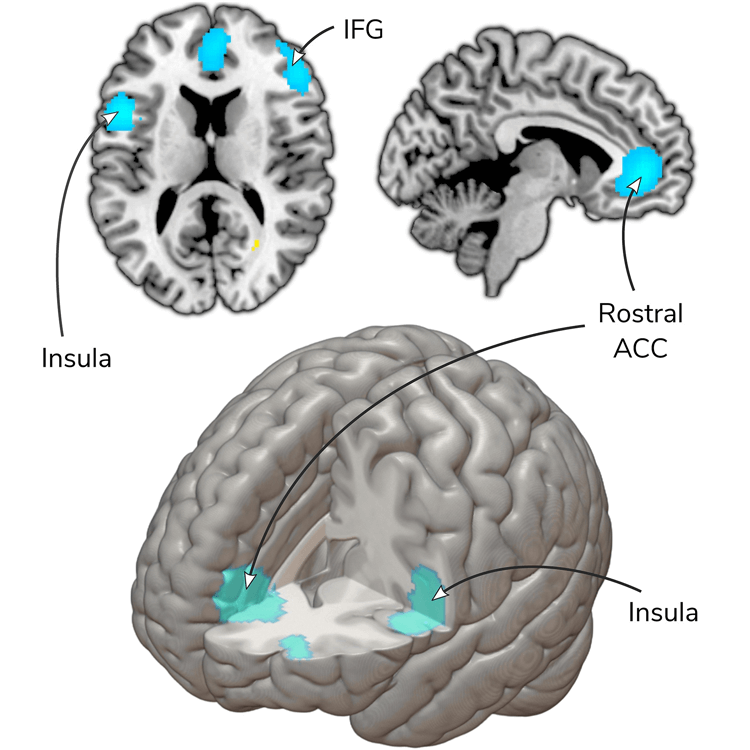
Analyzing results of 22 studies that scanned patients’ brains before and after undergoing therapy, researchers found some consistent changes in brain activity. Blue highlights indicate brain regions where activity decreased after therapy, including the cingulate cortex (rostral ACC) and insula, which are involved in emotional processing and anxiety. IFG refers to the inferior frontal gyrus, which is involved in language processing.
CREDIT: L. MARWOOD ET AL / NEUROSCIENCE & BIOBEHAVIORAL REVIEWS 2018
Others searching for concrete markers of a patient’s progress have been measuring neurochemical changes during therapy. “We don’t just ask the depressed patient if he’s feeling better,” says Sigal Zilcha-Mano, a clinical psychologist and expert on the patient-therapist bond at the University of Haifa in Israel. She and her team also measure levels of the stress hormone cortisol, the bonding hormone oxytocin, body temperatures, and the synchrony of speech and movement between patient and therapist.
These measurements, which capture changes many patients and therapists aren’t aware of in the moment, may eventually present a detailed portrait of what can be among the most intense of human relationships. One day, Zilcha-Mano says, they may also enable more precise, individualized, tailored treatments for each patient. It’s a matter of traits and states, she explains. Patients may come to therapy with the trait of being more or less able to trust and form relationships. But depending on the skill of the therapist, they may enter a state of being more open to such a bond. The real-time portrait of chemical changes and movements could someday illuminate this process, particularly in the case of oxytocin, considered to be an important biological marker of trust.
In whatever way it might happen, breaking through the current impasse over what makes psychotherapy effective could help practitioners do a better job, Cuijpers and his colleagues argue. Psychotherapeutic treatments for depression haven’t improved in decades, they note.
They also hope that more cogent explanations for how talk therapy works could help revive the approach, which other critics say has long suffered from a reputation of lacking scientific credibility.
“Understanding how therapies work,” write Cuijpers and his colleagues, “may make it possible to develop treatments that focus on the core processes and are, therefore, more effective and efficient, and more acceptable to patients.”
Skepticism about how psychotherapy works was a problem long before Freud came on the scene. It’s at least as old as the charismatic German physician Franz Anton Mesmer, born in 1734. His practice of “mesmerism” relied on claims that he could manipulate an invisible bodily fluid through “animal magnetism.” Mesmer established a strong rapport with his patients with nervous disorders, many of whom ended up feeling they had been cured.
But he alienated other doctors, and in 1784, while Mesmer was practicing in Paris, King Louis XVI appointed an international commission of scientists and physicians, including Benjamin Franklin, to investigate his methods. They concluded that he couldn’t support his claims of invisible fluids or animal magnetism, ruining his reputation.
Mesmer’s treatment worked — at least for some — but not his explanation of how it did so. Psychotherapy’s quest for legitimacy continues.




