Studies of migraine’s many triggers offer paths to new therapies
One class of drugs has already found success in treating the painful, disorienting and common attacks. Excitement is building about a slew of additional drug targets.
Support sound science and smart stories
Help us make scientific knowledge accessible to all
Donate today
For Cherise Irons, chocolate, red wine and aged cheeses are dangerous. So are certain sounds, perfumes and other strong scents, cold weather and thunderstorms. Stress and lack of sleep, too.
She suspects all of these things can trigger her migraine attacks, which manifest in a variety of ways: pounding pain in the back of her head, exquisite sensitivity to the slightest sound, even blackouts and partial paralysis.
Irons, 48, of Coral Springs, Florida, once worked as a school assistant principal. Now, she’s on disability due to her migraine. Irons has tried so many migraine medications she’s lost count — but none has helped for long. Even a few of the much-touted new drugs that have quelled episodes for many people with migraine have failed for Irons.
Though not all are as impaired as Irons, migraine is a surprisingly common problem, affecting 14 percent to 15 percent of people. Yet scientists and physicians remain largely in the dark about how triggers like Irons’s lead to attacks. They have made progress nonetheless: The latest drugs, inhibitors of a body signaling molecule called CGRP, have been a blessing for many. For others, not so much. And it’s not clear why.
The complexity of migraine probably has something to do with it. “It’s a very diverse condition,” says Debbie Hay, a pharmacologist at the University of Otago in Dunedin, New Zealand. “There’s still huge debate as to what the causes are, what the consequences are.”
That’s true despite decades of research and the remarkable ability of scientists to trigger migraine attacks in the lab: Giving CGRP intravenously to people who get migraines gives some of them attacks. So do nitric oxide, a natural body molecule that relaxes blood vessels, and another signaling molecule called PACAP. In mice, too, CGRP and PACAP molecules can bring on migraine-like effects.
All these molecules act as “on” switches for migraine attacks, which suggests that there must be “off” switches out there too, says Amynah Pradhan, a neuroscientist at Washington University in St. Louis. Scientists have been actively seeking those “off” switches; the CGRP-blocking drugs were a major win in this line of research.
Despite the insights gleaned, migraine remains a tricky disease to understand and treat. For example, the steps between the molecular action of CGRP and a person experiencing a headache or other symptoms are still murky. But scientists have lots of other ideas for new drugs that might stave off migraine attacks, or stop ongoing ones.
“It’s important to have an expanded toolbox,” says Pradhan.
Deciphering migraine mechanisms
Migraine is the second most prevalent cause of disability in the world, affecting mainly women of childbearing age. A person may have one migraine attack per year, or several per week, or even ongoing symptoms.
Complicating the picture further, there’s not just one kind of migraine attack. Migraine can cause headache; nausea; sensitivity to light, sound or smell; or a panoply of other symptoms. Some people get visual auras; some don’t. Some women have migraine attacks associated with menstruation. Some people, particularly kids, have “abdominal migraine,” characterized not so much by headaches as by nausea, stomach pain and vomiting.
Initially, the throbbing nature of the head pain led researchers to suspect that the root problem was expansion of the blood vessels within the membranes surrounding the brain, with these vessels pulsing in time with the heartbeat. But, as it turns out, the throbbing doesn’t really match up with heart rate.
Then researchers noticed that many signs that presage migraine attack, such as light sensitivity and appetite changes, are all regulated by the brain, particularly a region called the hypothalamus. The pendulum swung toward suspicion of a within-brain origin.
Today, scientists wonder if both in-brain and beyond-brain factors, including blood vessels releasing pain-causing molecules, play a role, as may other contributors such as immune cells.
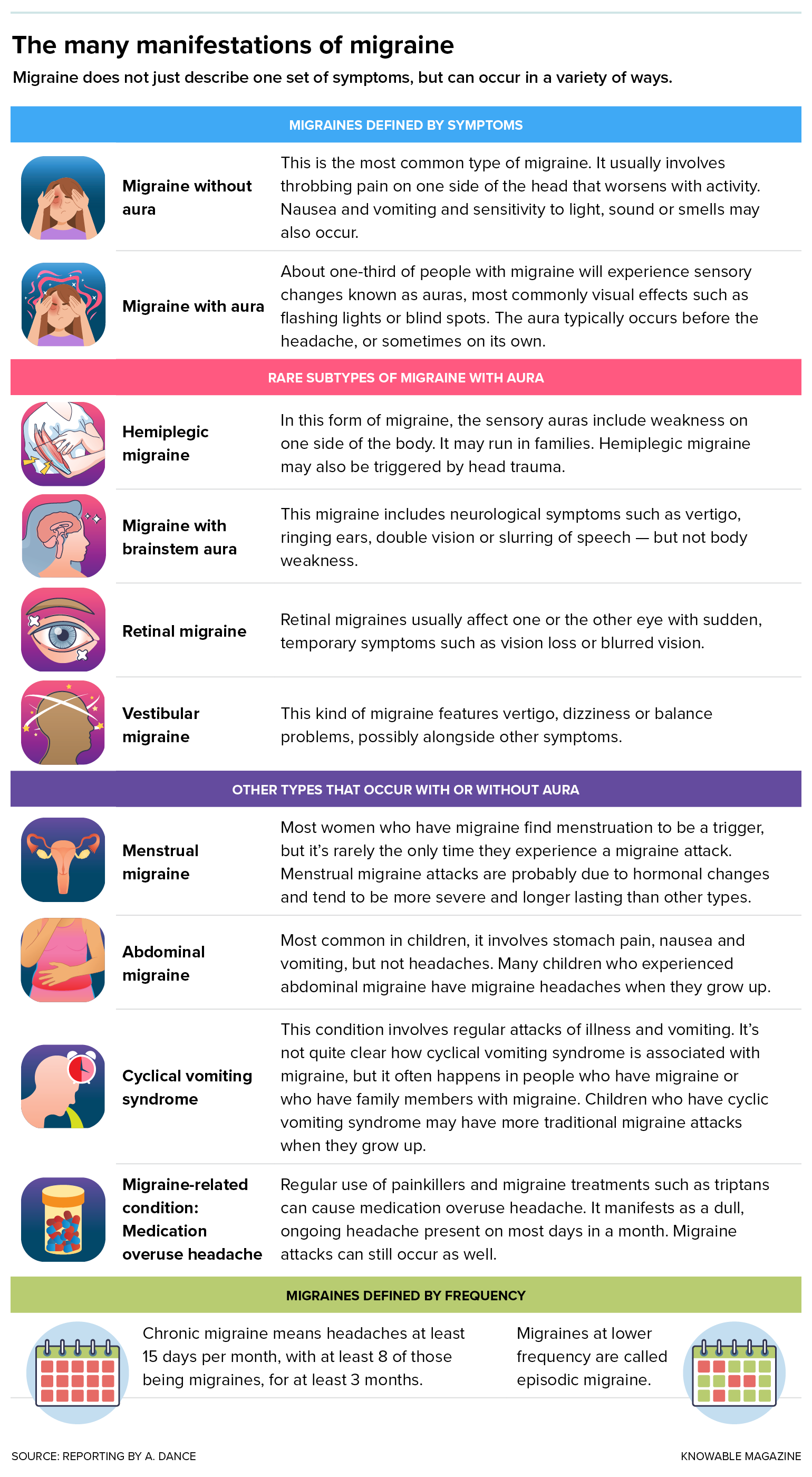
People may experience migraine in very different ways.
What all these proposed mechanisms ultimately point to, though, is pain created not in the brain itself but in the meninges — a multilayered “plastic bag around your brain,” as described by Messoud Ashina, a neurologist at the University of Copenhagen and director of the Human Migraine Research Unit at Rigshospitalet Glostrup in Denmark. These membranes contain cerebrospinal fluid that cushions the brain and holds it in place. They also support blood vessels and nerves that feed into the brain. The brain itself cannot feel pain, but nerves in the meninges, especially the trigeminal nerve between the face and brain, can. If they’re activated, they send the brain a major “ouch” message.
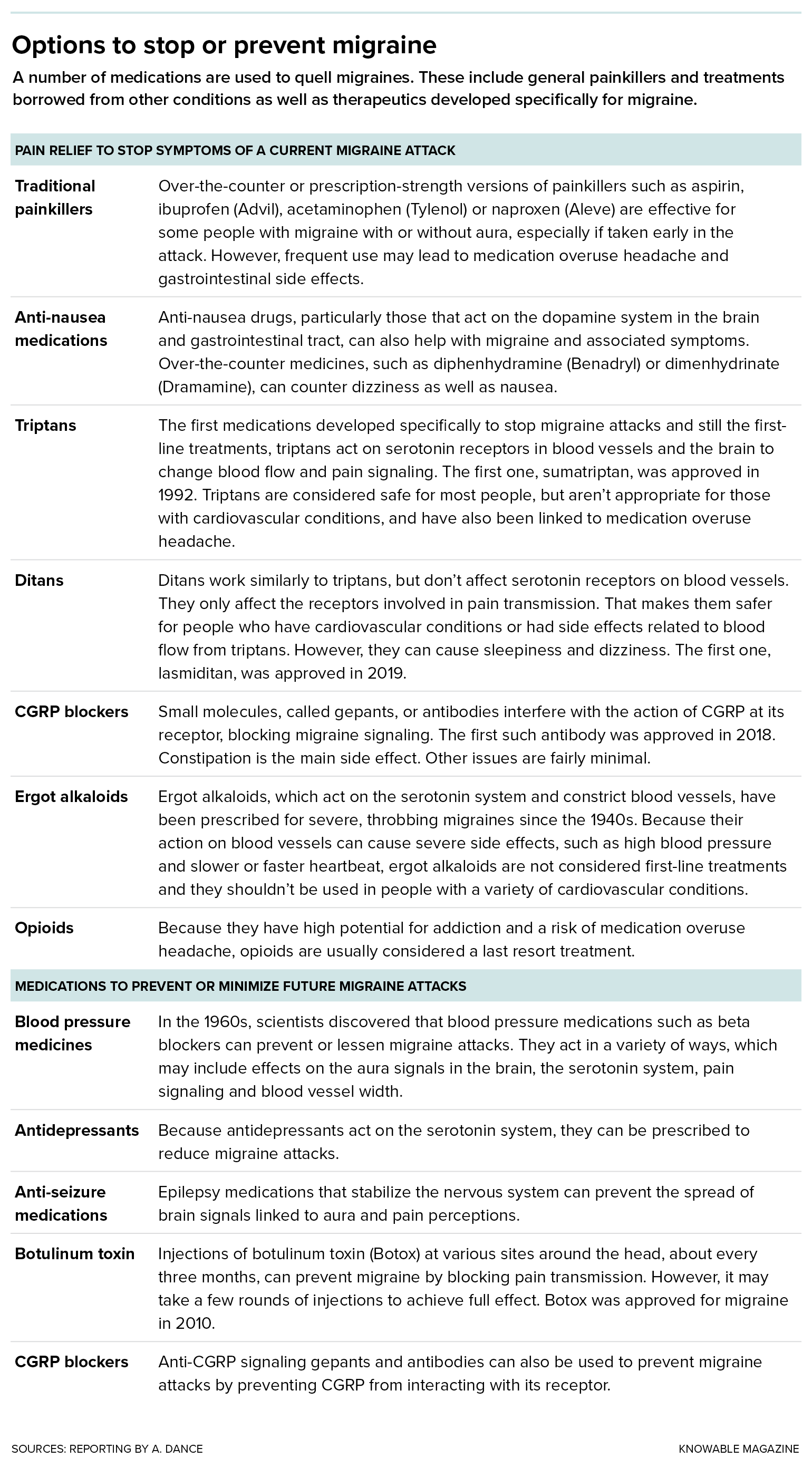
Physicians and pharmacists already possess a number of anti-migraine tools — some to prevent future attacks, others to treat an attack once it’s started. Options to stop a current migraine attack in its tracks include over-the-counter painkillers, such as aspirin and ibuprofen, or prescription opioids. Triptans, developed specifically to counter migraine attacks once they’ve begun, are drugs that tighten up blood vessels via interactions with serotonin receptors.
However, scientists later recognized that constricting blood vessels is not the main way triptans relieve migraine; their action to quiet nerve signals or inflammation may be more relevant. Ditans, a newer class of migraine drugs, also act on serotonin receptors but affect only nerves, not blood vessels, and they still work.
For migraine attack prevention, pre-CGRP-era tools still in use today include antidepressants, blood pressure medications, epilepsy drugs and injections of botulinum toxin that numb the pain-sensing nerves in the head and neck.
Most of these medicines, except triptans and ditans, weren’t designed specifically for migraine, and they often come with unpleasant side effects. It can take months for some preventive medicines to start working, and frequent use of triptans or painkillers can lead to another problem, the poorly understood “medication overuse headache.”
A powerful new player
The CGRP drugs provided a major expansion to the migraine pharmacopoeia, as they can both prevent attacks from happening and stop ones that have already started. They also mark the first time that clues from basic migraine research led to an “off” switch that prevents migraine attacks from even starting.
CGRP is a small snippet of protein made in various places in the body. A messenger molecule that normally clicks into another molecule, called a receptor, on a cell’s surface, CGRP can turn on activity in the receiving cell. It’s found in pain-sensing nerve fibers that run alongside meningeal blood vessels and in the trigeminal ganglia near the base of the skull where many nerves are rooted. The molecule is a powerful blood vessel dilator. It also acts on immune cells, nerve cells and the nerve-supporting cells called glia.
All of these features — a location in the meningeal nerve fibers with several actions that might be linked to migraine, like expanding blood vessels — pointed to CGRP being a migraine “on” switch. Further research also showed that CGRP is often found at higher levels in the body fluids of people who get migraines.
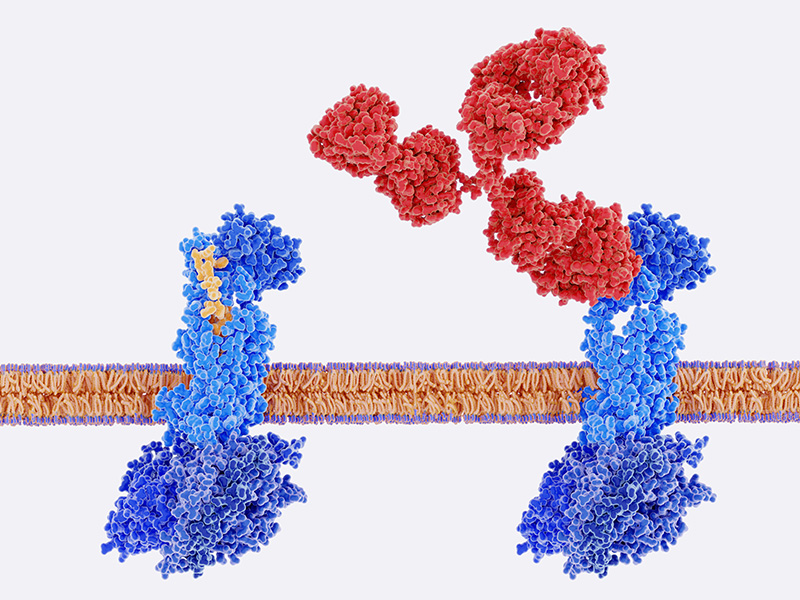
The CGRP receptors (blue) sit in the cell membrane (tan). On the cell’s exterior surface, CGRP (yellow) can bind to the receptor, kicking off signaling within the cell. But if an antibody (red) gets in the way, CGRP can’t reach its binding site on the receptor.
CREDIT: JUAN GAERTNER / SHUTTERSTOCK
In a small 2010 study, 12 out of 14 people with migraine did report a headache after receiving intravenous CGRP; four of them also experienced aura symptoms such as vision changes. Only two out of 11 people who don’t normally get migraine attacks also developed a headache after CGRP infusion.
CGRP also caused mice to be extra sensitive to light, suggesting it could have something to do with the light sensitivity in humans, too.
The steps between CGRP in the bloodstream or meninges as a trigger and migraine symptoms like light sensitivity aren’t fully understood, though scientists do have theories. Ashina is pursuing how CGRP, PACAP and other substances might trigger migraine attacks. These molecules all stick to receptors on the surface of cells, such as the ones in blood vessel walls. That binding kicks off a series of events inside the cell that includes generation of a substance called cyclic AMP and, ultimately, opening of channels that let potassium ions out of the cell. All that external potassium causes blood vessels to dilate — but it might also trigger nearby pain-sensing nerves, such as the trigeminal cluster, Ashina hypothesizes.
It’s a neat story, but far from proven. “We still don’t really know what CGRP does in the context of migraine,” says Greg Dussor, a neuroscientist at the University of Texas at Dallas.
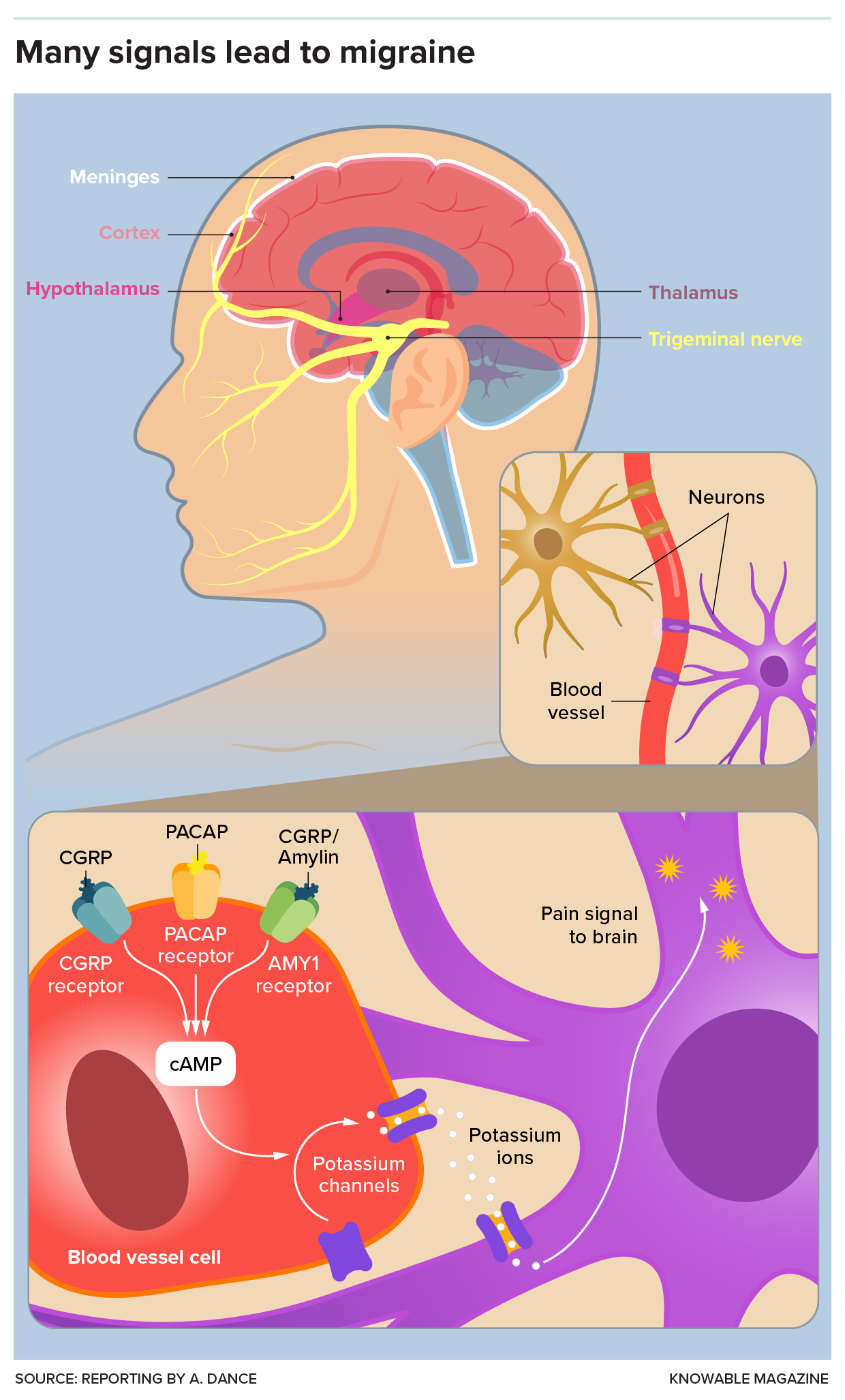
In one possible model for migraine, various molecules can activate blood vessel cells to release potassium, which activates nearby neurons that send a pain signal to the brain. Various strategies that seek to interfere with this pathway, including the anti-CGRP drugs, are of great interest to migraine researchers.
Uncertainty about CGRP’s precise role in migraine hasn’t stopped progress in the clinic: There are now eight different blockers of CGRP, or its receptor, approved by the US Food and Drug Administration for migraine treatment or prevention. The American Headache Society recently released a statement saying that CGRP drugs should be considered first-line treatments for migraine. Despite CGRP’s widespread presence across the body, blocking it results in few and generally mild side effects, such as constipation.
“It’s a good drug,” says Dan Levy, a neurophysiologist at Beth Israel Deaconess Medical Center in Boston who recently described the role of the meninges in migraine for the Annual Review of Neuroscience.
Questions remain, though. One is whether, and how well, CGRP blockers work in men. Since three to four times as many women as men have migraine, the medicines were mostly tested in women. A recent review found that while CGRP blockers seem to prevent future headaches in both sexes, they haven’t been shown to stop acute migraine attacks in men as currently prescribed. (Notably, men made up less than a fifth of those included in the studies as a whole, making it more difficult to detect any low-level effects.)
More data may settle the question. Hsiangkuo Yuan, neurologist and director of clinical research at Thomas Jefferson University’s headache center in Philadelphia, says he’s been tracking effects of CGRP blockers in his patients, and hasn’t seen much difference between the sexes so far in terms of CGRP-blocking antibodies, though there may be a difference in how people respond to small molecules that block CGRP.
Access to CGRP inhibitors has also become an issue. Many insurers won’t pay for the new drugs until patients have tried and failed with a couple of other treatments first — which can take several months. This led Irons, the Florida patient, to try multiple medications that didn’t help her before she tried several CGRP blockers. In her case, one CGRP drug didn’t work at all; others worked for a time. But eventually they all failed.
Searching for new “off” switches
Her case illustrates the need for still more options to prevent or treat migraine attacks, even as the CGRP success story showed there’s hope for new medicines.
“CGRP has really paved the way,” says Andrew Russo, a neuroscientist at the University of Iowa in Iowa City who described CGRP as a new migraine target for the Annual Review of Pharmacology and Toxicology in 2015. “It’s a very exciting time for the field.”
Physicians have a number of therapies that can treat migraine — from familiar painkillers such as acetaminophen to the newer ditans and CGRP blockers. Yet, many patients still struggle to find consistent symptom relief, motivating scientists to continue to search for new medications.
Russo and Hay, of New Zealand, are interested in building on CGRP action with a potential novel therapy. It turns out CGRP doesn’t hit just one receptor on the surface of cells, like a key that matches only one lock. In addition to the traditional CGRP receptor, it also binds and activates the AMY1 receptor — which itself can be activated by another molecule, amylin.
AMY1 receptors are found at key sites for migraine pain, such as the trigeminal nerves. In a small study, Russo and Hay found that injecting a synthetic version of amylin creates migraine-like attacks in about 40 percent of people with migraine. The researchers also discovered that in mice, activating AMY1 causes sensitivity to touch and light.
Again, that sounds like a migraine attack “on” switch, and Russo believes there’s a good chance that researchers can develop a drug that acts as an “off” switch.
Another promising “on” switch contender is PACAP. Like CGRP, it’s a small protein and signaling molecule. PACAP also appears in the trigeminal nerves that transmit migraine pain, and seems to be elevated in some people experiencing a migraine attack. In rodents, PACAP causes expansion of blood vessels, inflammation in the nervous system and hypersensitivity to touch and light. In a little over half of people with migraine, intravenous PACAP kicked off a fresh, migraine-like attack.
But, Russo says, “PACAP is more than just a CGRP wannabe.” It appears to work at least somewhat differently. In mice, antibodies that block PACAP do nothing against the light aversion activated by CGRP, and vice versa. That suggests that PACAP and CGRP could instigate two alternate pathways to a migraine attack, and some people might be prone to one or the other route. Thus, PACAP-blocking drugs might help people who don’t get relief from CGRP blockers.
Clinical research so far hints that anti-PACAP treatments indeed might help. In 2023, the Danish pharmaceutical company Lundbeck announced results of a trial in which they dosed 237 people with an antibody to PACAP. Those who received the highest dose had, on average, six fewer migraine days in the four weeks following the treatment than they did before receiving the medication, compared to a drop by only four days in people who received a placebo.
Then there’s Ashina’s work, which unites many of the “on”-switch clues to suggest that PACAP, CGRP and other molecules all act by triggering cyclic AMP, causing blood vessel cells to spew potassium. If that’s so, then drugs that act on cyclic AMP or potassium channels might serve as “on” or “off” switches for migraine attacks.
Ashina has tested that hypothesis with cilostazol, a blood vessel dilator used in people who have poor circulation in their legs. Cilostazol boosts production of cyclic AMP and, Ashina found, it caused attacks in a majority of people with migraine.
He also tried levcromakalim, another blood vessel opener that lowers blood pressure. It’s a potassium-channel opener, and this, too, caused migraine attacks for all 16 people in the study.
To Ashina, these experiments suggest that medicines that turn off migraine-inducing pathways at or before the point of potassium release could be of benefit. There might be side effects, such as changes in blood pressure, but Ashina notes there are potassium-channel subtypes that may be limited to blood vessels in the brain. Targeting those specific channels would be safer.
“I personally really like the potassium-channel track,” says Russo. “I think if we can find drugs targeting the ion channels, the potassium channels, that will be fruitful.”
Hopeful for opioids
Russo is also upbeat about work on a new kind of opioid. Traditional opioids, whether from poppies or pharmacies, work on a receptor called mu. Along with their remarkable pain-dulling abilities, they often create side effects including constipation and itching, plus euphoria and risk for addiction.
But there’s another class of opioid receptors, called delta receptors, that don’t cause euphoria, says Pradhan, who’s investigating them. When delta-targeting opioid molecules are offered to animals, the animals won’t self-administer the drugs as they do with mu-acting opioids such as morphine, suggesting that the drugs are less pleasurable and less likely to be habit-forming.
Delta receptors appear in parts of the nervous system linked to migraine, including the trigeminal ganglia. Pradhan has found that in mice, compounds acting on the delta opioid receptor seem to relieve hypersensitivity to touch, a marker for migraine-like symptoms, as well as brain activity associated with migraine aura.
Encouraged by early evidence that these receptors can be safely targeted in people, two companies — PharmNovo in Sweden and Pennsylvania-based Trevena — are pursuing alternative opioid treatments. Migraine is one potential use for such drugs.
Thus, the evolving story of migraine is one of many types of triggers, many types of attacks, many targets, and, with time, more potential treatments.
“I don’t think there’s one molecule that fits all,” says Levy. “Hopefully, in 10, 15 years, we’ll know, for a given person, what triggers it, and what can target that.”
Editor’s note: This story was updated on October 17, 2024, to correct the name of the University of Texas at Dallas.
10.1146/knowable-101424-1
TAKE A DEEPER DIVE | Explore Related Scholarly Articles






