Call it the body’s postal system. Cells package goodies into little envelopes made of membranes. Then these packages cruise the bloodstream — billions of them in every milliliter of blood — to recipient cells far and near, delivering freight such as genetic material and proteins.
These little bubbles, known as extracellular vesicles, or EVs, tell the receiving cell to change its biology, with far-reaching consequences, potentially influencing how we learn, the timing of childbirth, where diseases like cancer spread to, and more.
Scientists first caught a glimpse of EVs in the 1940s, and when researchers studied them in more detail in the 1980s, they thought they were looking at mundane cellular trash bags. Then, a couple of decades later, a team of interdisciplinary researchers discovered that tumors send EVs to distant tissues, laying the groundwork for cancer to take hold in new places. Today, scientists are finding that the messages EVs deliver are important in multiple sites around the human body, both in health and sickness. Cells of animals and plants, protozoans and fungi, and even bacteria release EVs, mailing their messages to other organs or other creatures they’re interacting with.
The cellular packages called exosomes have membranes studded with various sets of proteins, fats and other particles (center). Ranging from 30 to 100 nanometers across, exosomes travel to distant cells in a variety of body fluids.
EVs are a mixed bag; scientists are still finding new varieties and figuring out how to categorize them. Different types originate in different cellular packaging plants. They vary in size from 20 to 1,000 nanometers, or up to about one-thousandth of a millimeter. On the smaller side, types called exosomes are created inside specialized cellular factories and then exported. Others that pinch off from a cell’s own membrane are called microvesicles or ectosomes, and tend to be larger.
The contents vary too, but one frequent cargo is small molecules of RNA — snippets of genetic material that can turn genes on or off in the cells they are dispatched to.
In many cases, scientists are just starting to figure out how the cells that send out EVs package their specific cargoes, what those cargoes are and how the EVs influence the cells where they end up. Medical applications are under investigation too, by companies like Codiak BioSciences, ReNeuron, Exosomics and Exosome Sciences. Specific EVs found in body fluids might help doctors diagnose diseases, for example, and lab-created EVs might package and deliver drugs to therapeutic targets.
Here’s a taste of some of the things that EVs do — and how scientists could harness them for novel purposes.
EVs known as exosomes are generated in a special cellular depot called the multivesicular body and sent out for delivery to recipient cells, which can take up the contents or the entire vesicle and use the proteins or genetic material inside.
EVs in cancer: A tool for tracking
David Lyden, a cancer biologist at Weill Cornell Medicine in New York, studies how cancer spreads from one tumor to other parts of the body — say, when a melanoma in the skin sends out cells to set up shop in the lungs and form a secondary malignancy.
Working with mice that had melanoma, Lyden and colleagues first used a technical trick to tag blood cells and tumor cells so they glowed green and red, respectively. Observing the mice over time, they noticed that the green blood cells got to the lungs before the red tumor cells arrived there, findings reported in Nature in 2005. Moreover, as described in 2012 in Nature Medicine, the team saw tiny red specks joining those blood cells early on, indicating that the tumors were sending in EVs to prepare the area. EVs seem to build up blood flow, change immune responses and remodel the environment outside cells to better support the incoming cancer cells.
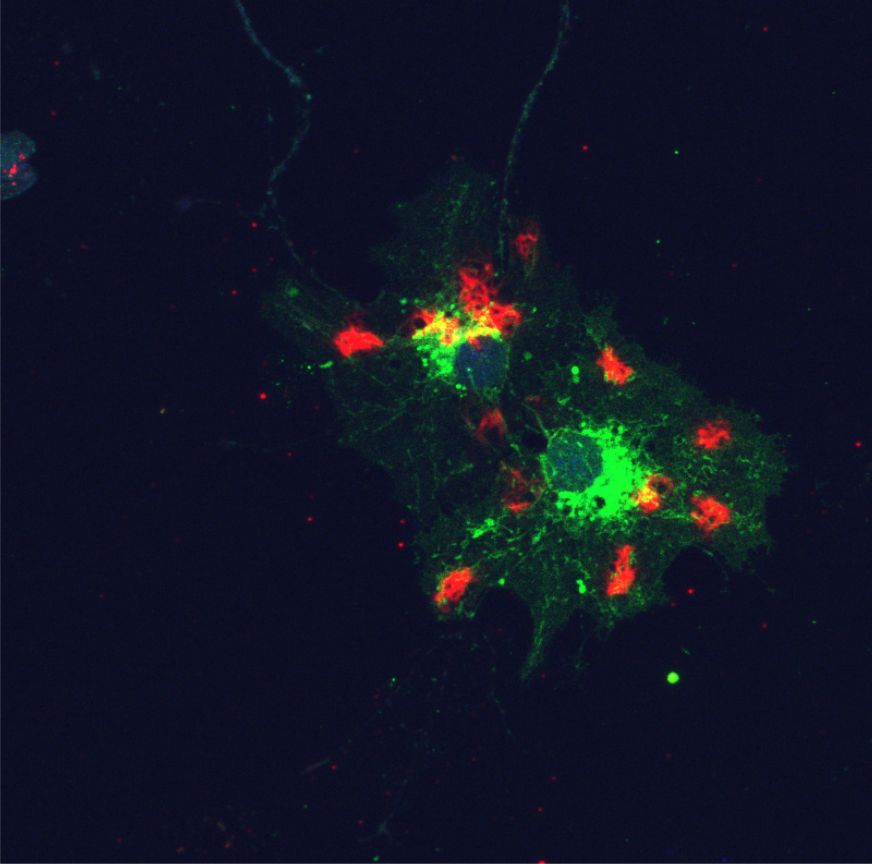
Cells from mouse connective tissue take up human-derived EVs (green) and concentrate them around the nucleus (blue); part of the cellular skeleton (red) is also visible. Many cells in the body make EVs, including tumor cells, so tracking the spread of EVs could help with the targeting of cancer therapies.
CREDIT: AYUKO HOSHINO AND DAVID LYDEN
The team also analyzed EVs extracted from the blood of people with advanced melanoma. They discovered that EVs from tumors carried a complement of proteins, fats and genetic material entirely distinct from vesicles coming from healthy tissues.
EVs could help doctors diagnose and track cancer, as well as predict if it will spread. One of Lyden’s collaborators, Johan Skog, cofounded Exosome Diagnostics, a company that has developed urine and blood tests for cancer-derived vesicles. For example, if patients have tumors removed but still have cancer EVs in their blood, it would suggest there’s still some cancer around, sending out seeds for its next move. The patients could then receive more aggressive treatment.
EVs from parasites: Preparing a niche?
Trypanosomes are slug-shaped protozoans that cause African sleeping sickness. Transmitted by the bite of the tsetse fly, they cause fevers, rashes and anemia, followed by seizures, personality changes and daytime sleepiness as the illness worsens.
Trypanosomes have tail-like structures, but scientists didn’t think much about those tails until recent work by the lab of Stephen Hajduk, a biochemist at the University of Georgia in Athens. “They actually look like beads on a string,” Hajduk says. When the beads reach the end of the string, they pinch off and float away as EVs called ectosomes, Hajduk’s group reported in the journal Cell in 2016.
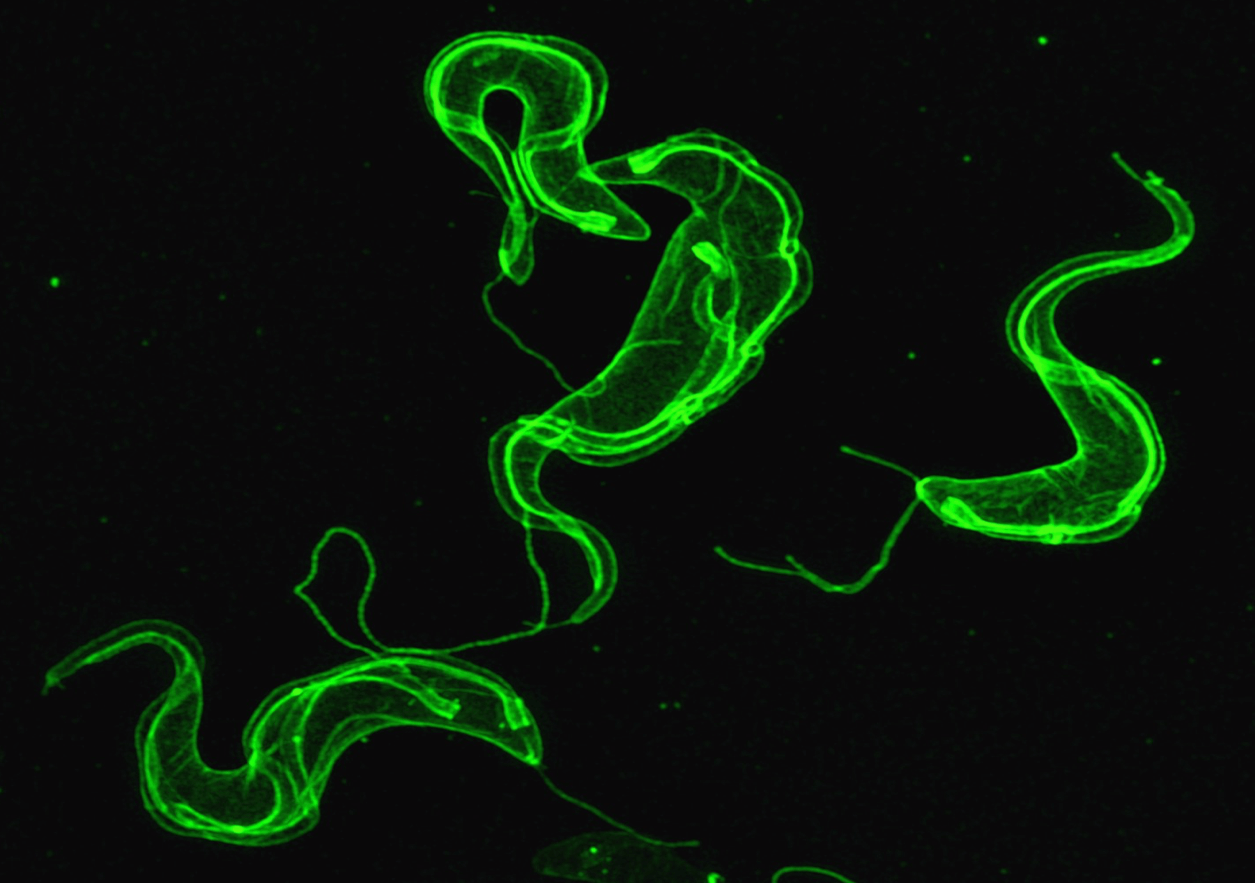
A super-resolution microscope image of three trypanosomes, the cause of African sleeping sickness. The parasites may use EVs to prepare their favorite body niches for invasion.
CREDIT: JUSTIN WIEDEMAN
Hajduk isn’t sure what the EVs do for the trypanosomes in infected people, but he thinks they act much like tumor EVs, preparing far-off regions of the body for future colonization, in this case by the parasite. To nail down that theory, he’s working in mice to see if the ectosomes reach sites where trypanosomes like to settle: the reproductive organs, fat tissue and the brain. He’s also collaborating with the US Centers for Disease Control and Prevention to use trypanosome EVs as a potential means to diagnose sleeping sickness.
EVs may also explain why trypanosomes cause anemia. The researchers found that the ectosomes fuse with red blood cells, making their membranes less flexible. Immune cells, scouting for broken-down old blood cells, recognize this membrane rigidity as a sign of aging and clear the cells away.
EVs on your mind: Sharing memories
The brain has its own EVs. At the University of Utah in Salt Lake City, neuroscientist Jason Shepherd studies a gene called Arc, which carries instructions for a protein that’s key for long-term memory. His team reported in Cell in 2018 that this Arc protein assembles to form containers similar to the shells of viruses. Once assembled, these structures pop out of nerve cells, picking up a membrane coat along the way.
“This was a real surprise,” recalls Shepherd. He wasn’t expecting a gene in nerve cells to make something that looked like a virus. “It’s kind of a crazy biology.”
The team also found that these Arc EVs carry RNAs inside them — ones bearing instructions to make the Arc protein itself, and perhaps others — that seem to be used by the cells that take them up. Given Arc’s known function in memory and the ability of EVs to transfer materials from cell to cell, he suspects that the Arc-based EVs help nerve cells communicate with each other so that memories can form.
Shepherd is also investigating other, unshelled, EVs in the brain. These can cause problems, too, in diseases such as Alzheimer’s and Parkinson’s, where cells fill up with toxic, malformed proteins. “The garbage disposal is sort of blocked, or it can’t work anymore,” Shepherd says. EVs may then carry the dangerous proteins from cell to cell, across the nervous system, bringing the disease along with them.
EVs in a glass of milk: They do a body good
The average American drinks 17 gallons of milk every year, and it’s packed with cow exosomes that have the potential to make their mark on human biology. Janos Zempleni, director of the Nebraska Center for the Prevention of Obesity Diseases at the University of Nebraska-Lincoln, and colleagues described the exosome component of milk in 2019 in the Annual Review of Animal Biosciences. In one study, Zempleni tested the blood of people after they drank milk and found cow RNAs there. The group reported in 2014 in the Journal of Nutrition that some of these RNAs control a human gene involved in making bone cells. So it’s possible they could influence skeletal growth.
Zempleni went on to genetically engineer mother mice so they couldn’t make milk exosomes. Their nursing pups weighed 25 to 30 percent less than pups getting exosome-loaded milk, he says.
Many milk exosomes end up in the brain, where they appear to influence thinking. Mice on a low-exosome diet can take up to twice as long to find the exit to a maze, compared to ones fed exosomes, Zempleni’s team reported in the FASEB Journal in 2017. “They really have a very, very poor performance in any test related to spatial learning and memory,” he says — though the mice do catch up in mental skills as they grow.
Incorporating a fluorescent tag into genetic material allowed researchers to follow the fate of glowing exosomes delivered via breast milk from mother mice to their pups’ organs, such as the brain and liver (left). Organs from a control mouse pup, without such genetic tagging, are also shown (right).
CREDIT: JANOS ZEMPLENI AND BIJAYA UPADHYAYA, U OF NEBRASKA LINCOLN
So what does this mean for the human infant diet? Zempleni and other researchers have tested formulas made from either soybean or cow milk proteins, and neither contained many exosomes, he says. Still, he suspects that children in developed nations get such rich nutrition that any exosome deficiency doesn’t make much of a difference to long-term brain development. But a lack of exosomes might be a problem for children in developing nations.
EVs in pregnancy: Bringing babies to term
Speaking of babies, exosomes have key roles in childbirth as well.
At the University of Texas Medical Branch in Galveston, reproductive biologist Ramkumar Menon is trying to understand how the fetus signals to the mother that it’s time to come out.
The membranes surrounding a fetus begin to age as the end of term approaches. They release exosomes, filled with cellular garbage, that incite inflammation in the mother.
Those junk-filled exosomes are enough to cause labor, Menon’s team reported this year in Scientific Reports. In mice, pregnancy lasts for 19 to 20 days. The researchers collected exosomes from the blood of mice that had been pregnant for 18 days — close to term — and injected them into mice that were 15 days pregnant. “And boom, they went into preterm labor,” typically delivering a day or two earlier than normal, Menon says.
Menon hopes that this work could lead to exosome-based tests for women at risk for preterm labor, or treatments to prevent preterm birth.
EVs in your heart: Delivering the goods
Cardiologist and researcher Eduardo Marbán also has treatments in mind: He wants to repair people’s tickers after heart attacks. He hoped that stem cells — blank-slate cells that can develop into a broad variety of tissues — would be able to rebuild heart muscle. And indeed, cardiac stem cells did help build up heart tissue after scientists in Marbán’s lab, at Cedars-Sinai Medical Center in Los Angeles, induced heart attacks in mice.
But when the researchers looked more closely, in a 2011 study in the journal Circulation, they saw that most of the stem cells disappeared within weeks, though the benefits lasted months. The timing wasn’t adding up. The team eventually figured out, and noted in Stem Cell Reports in 2014, that the stem cells released EVs containing RNAs that helped heart muscle and blood vessels grow. Based on these and other results, Marbán cofounded a company, Capricor Therapeutics, to develop exosomes as delivery vehicles for medicines. He and his Capricor colleague Ahmed Ibrahim summarized the state of exosome research in the cardiovascular system in the Annual Review of Physiology in 2016.
Scientists envision using EVs derived from stem cells as medicine-delivery vehicles. Large quantities of ready-to-use vesicles could be used to treat any patient (top), or EVs could be harvested from specific patients, their contents customized and then delivered back to that patient (bottom).
In another recent study in Stem Cell Reports, Marbán’s group used EVs to treat heart failure in mice engineered to mimic the muscle-wasting disease Duchenne muscular dystrophy. Not only did the EVs help the heart work better, they also helped skeletal muscles.
EVs loaded with therapeutic cargos would be much easier to use as a treatment than stem cells, Marbán says. They could deliver RNAs, genes, proteins —whatever scientists load them with. Unlike most stem cells, the EVs can be freeze-dried for convenient storage. And they can cross into the brain, making them potential delivery trucks to treat neurological conditions such as Alzheimer’s.
EVs in plants: Killing invaders
Plants make EVs, too. They appear to use them for defense, fighting off fungi and bacteria.
Roger Innes, a plant biologist at Indiana University in Bloomington, has collected EVs from the leaves of Arabidopsis, a relative of mustard and broccoli that scientists often use in the lab. The EVs were full of proteins that plants manufacture to respond to infections and other stressful situations, Innes and his student Brian Rutter reported in the journal Plant Physiology in 2017.
These EVs stick to fungi, and the fungal cells take them up. That can be a fatal mistake, because some of the cargoes seem to comprise a two-part anti-fungus poison. Innes has evidence that some EVs contain chemicals called glucosinolates, which are harmless on their own. Other EVs hold enzymes that act like molecular scissors, slicing those glucosinolates in half. That slicing produces a killer molecule that prevents fungal cells from making energy, so they die. (Glucosinolates are also responsible for the characteristic odor of plants like mustard and broccoli.)
To take advantage of plant EVs, scientists might engineer them to carry small RNAs that would improve crops’ resistance to pests and disease, Innes says. He also sees applications for plant EVs in medicine, because animals can take up EVs from the plants they eat. He thinks it would be easier and cheaper to engineer plants to make therapeutic EVs, and to grow entire fields full of medicinal crops, than to make drug-toting EVs in a lab.
Address unknown
But before we get to enjoy salads laden with beneficial EVs, scientists have a long way to go. Researchers don’t fully understand how cells shunt specific cargoes into EVs as they’re made. In many cases, they still don’t know what those cargoes are, and how they influence the cells that receive and open the packages.
Another major mystery is how these vesicles are addressed so they’re delivered to the right cell recipients. Researchers do know that some exosomes are studded with proteins that hook up with ones on the membranes of target tissues. To create therapeutic EVs, Marbán and others are working on ways to put artificial addresses on the vesicles, modifying their membranes so they find the right place in the body.
Though EV research is just getting started, it has already built a picture of a bloodstream packed with letters and packages of diverse sizes bobbing along in the flow, somehow finding their addressees amid the chaos. It’s like the most hectic post office on the day before Christmas — all day and all night, all over our bodies.




