Q&A — Immunologist and cancer researcher Özlem Türeci
After Covid-19, can mRNA vaccines help with cancer as well?
The pandemic put the technology, long in development, to the test. Here’s a look at the status of its application to cancer and when it might reach patients.
Support sound science and smart stories
Help us make scientific knowledge accessible to all
Donate today
Vaccines against Covid-19 were delivered with remarkable and unprecedented speed. The ones pioneered by Moderna in the US and BioNTech in Germany introduced the lay public to a new kind of shot: one that includes mRNA, the nucleic acid that normally carries genetic instructions from the cell nucleus to the part of the cell where proteins are made.
How could this novel technology have come together so rapidly?
In fact, the approach had long been in the works, although it was not initially intended to prevent viral disease. Rather, it was focused on treating cancer, explains Özlem Türeci, cofounder and chief medical officer of BioNTech, the company that developed the Covid-19 vaccine with Pfizer.
The anti-cancer rationale goes like this: Since each tumor contains a multitude of genetic mutations that do not occur elsewhere in the body, this should in theory allow our immune system to recognize and destroy those cells. Alas, tumors are known to suppress the immune system. In response, scientists have developed various drugs and treatments to stimulate the immune system in cancer patients.
But another problem is that many tumor mutations slip through the net. So some researchers have proposed a more focused approach to alert immune cells to cancer mutations they do not spontaneously target — something more like a vaccine, which usually works by exposing people to an inactivated pathogen or some of its signature molecules. This primes the immune system for immediate action should the active pathogen show up. In a similar vein, the scientists reasoned it might be possible to present the patient’s immune system with specific bits of cancer tissue, to train it to attack the tumor more vigorously.
The benefit of using mRNA for this job is not just that it can be manufactured relatively quickly, but that it is also very flexible. The genetic signature of a tumor is different in every person and, as time progresses, it continues to change. This means that vaccines would ideally be tailor-made, and repeatedly so — an expensive and time-consuming proposition if one is manufacturing bits of key tumor protein in the lab, which was a very common way of producing vaccines before mRNA arrived. Proteins are built from a score of different amino acids, have complicated three-dimensional structures and tend to clump together when something goes wrong.
So, what if we could just make specific pieces of mRNA instead, inject them into the body, and let the cells build the corresponding proteins themselves? Wouldn’t that be much easier?
In the approach BioNTech developed, explains Türeci, mRNA can be injected into the body and targeted towards the lymph nodes, where it is translated into protein by immune cells known as dendritic cells. These cells then display the protein on their surfaces, where they train the T cells that patrol our tissues to find and eliminate any intruders that display the same signature.
This schematic illustrates how an mRNA vaccine can help the body fight cancer cells. The mRNA carries instructions for making little pieces of protein that are produced by tumor cells. When the mRNA is taken up by dendritic cells of the immune system, the protein pieces (antigens) are produced and displayed on the surface of the dendritic cells. This display trains T cells to respond to the new antigen with an attack against the tumor. In a natural situation, the tumor itself releases bits of cancer debris (shown as little brown blobs) that are taken up by dendritic cells to train T cells. However, the immune system doesn’t react to all kinds of tumor antigens. The mRNA vaccine can train the body to target tumor antigens it normally doesn’t respond to. The result is a more effective attack against cancer cells.
The Covid-19 pandemic put the strategy to the test: Within a year, two highly effective mRNA vaccines against the SARS-CoV-2 virus were developed, tested and rolled out — one from Pfizer-BioNTech, one from Moderna, each slightly different. Both vaccines contained the code for making a stabilized version of the spike protein that the virus uses to get into cells. The spike protein code was inserted into mRNA with a backbone that had been optimized by decades of research. This mRNA was then packaged in specific lipids to ensure it would reach its lymph-node destination.
Türeci, who coauthored an article about mRNA vaccines against cancer for the Annual Review of Medicine in 2019, recently talked with Knowable Magazine about the development of mRNA vaccines for cancer and how close they are to reaching patients, for whom new therapies are sorely needed.
This conversation has been edited for length and clarity.
When did you start developing cancer vaccines, and why did you think mRNA would work best?
This did not happen overnight. It was a decades-long journey that started in the 1990s. We had a vision that was considered science fiction at the time: We wanted to develop cancer vaccines to shrink tumors. Every patient’s cancer is unique, because it is the result of random mutations, so we wanted to develop individualized vaccines that would activate the patient’s immune system against their own tumor.
We tested various approaches and identified mRNA as the one with the highest potential for the purpose of developing truly individualized cancer vaccines. Synthetic mRNA is produced by a simple process, and it looks very much like natural mRNA. It delivers the blueprint of the protein — the vaccine antigen — for the body’s cells to produce.
Yet we also realized that significant improvements would be needed. Over the past decades, we have addressed these shortcomings.
Our discoveries led to the mRNA technology platform that we use today for our product candidates against cancer, infectious diseases and other severe diseases. In addition to our own research in the 1990s, a small group of other scientists also worked on mRNA. Our advances as well as theirs provided the tailwind for the broader scientific community.
What have been the most crucial breakthroughs that allowed you to get to this point?
The fundamental problem of mRNA was its low potency. Even large doses of mRNA produce little protein and, consequently, had little effect. That is why, in the late 1990s, few in the industry believed in mRNA as a new class of drugs; mRNA vaccines tested at that time elicited poor immune responses.
Our team spent years researching each element of the mRNA backbone and discovered various modifications that increased the stability of the mRNA and its translation into protein. This way, we created mRNA backbones with a more than thousandfold increased efficacy to trigger immune responses.
The next piece of the puzzle was to find out how to get the mRNA vaccine to the right cells in the body, and which cells these might be. In 2004, we made an interesting observation: The direct injection of an mRNA vaccine with our improved backbone into a lymph node elicited a much stronger immune response than injection of mRNA into the skin or muscle, which were the commonly explored routes.
Why would it be so much more effective to inject the mRNA directly into the lymph nodes?
We realized that directing mRNA vaccines into dendritic cells in the lymph nodes had to become a critical part of the solution. In the years that followed, we explored various methods to deliver mRNA to these specific locations in the body, and discovered that mRNA vaccines encapsulated in a particular lipid nanoparticle — a technology we have developed and that we call RNA lipoplexes — were specifically taken up by resident dendritic cells in lymphoid tissues.
These cells are the high-performance trainers of the immune system and can mediate particularly strong immune responses. We found that they have a specific mechanism to engulf foreign bodies and use them to train the immune system. Vaccine-induced T-cell responses were extremely strong and eradicated large tumors in mice. So, with these discoveries and optimizations of our technology, we went back to the bedside, to the patient.
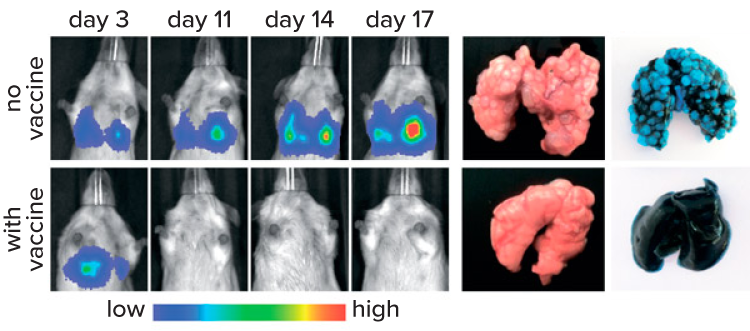
These images display the results of an mRNA vaccine experiment in mice. On the left are images of lung tumor tissue over time. The tumors consist of cancer cells that were engineered to be bioluminescent. In control animals that did not receive the mRNA vaccine, the tumors continued to grow. In animals that received the vaccine, the tumors shrank and were often no longer detected at 11 days or later. The pictures on the right show the lungs of mice that didn’t (top) or did (bottom) receive the vaccine. The lungs are stained with ink, then the tumor tissue was selectively bleached, resulting in a light blue color for tumor tissue.
CREDIT: ADAPTED FROM L.M. KRANZ ET AL / NATURE 2016
How exactly did you make the step from humans to mice?
We started human studies and pioneered, in 2015, the first systemic delivery of mRNA nanoparticle vaccines to humans. In a portion of our patients with treatment-resistant melanoma, we could observe shrinkage of tumors with the vaccine, alone or in combination with immune-stimulating medication. We published these findings in the journal Nature in 2017. They provided the blueprint for the development of highly effective mRNA vaccines.
These advances allowed us to come closer to our original vision of cancer vaccines tailored to the patient’s tumor. The approach involves genomic analysis of a patient’s tumor by next-generation sequencing to find the cancer-specific mutations by comparison to the patient’s normal tissue. This set of cancer mutations is unique for every patient. We then select a number of mutations that provide the highest likelihood for the immune system to recognize the cancer and design a vaccine tailored to the patient’s individual cancer mutation profile.
How many people have been treated with your mRNA cancer vaccines so far?
With our individualized vaccine candidates, we have treated more than 450 patients. These are designed to target mutations that are unique to the patient’s specific cancer. We also have a number of personalized off-the-shelf mRNA cancer vaccine candidates. These candidates consist of a fixed combination of mRNA-encoded non-mutated tumor antigens that are known to frequently be produced within specific cancer types. We are currently investigating these candidates in clinical studies — for example, in patients with advanced melanoma, prostate cancer or head and neck cancer — and have treated more than 250 patients so far.
This has all been in the context of clinical trials. The way treatments are developed within the regulatory framework is to go cancer by cancer, and independently for every line of treatment, for every cancer.
Our oncology pipeline currently counts 20 programs in 24 ongoing clinical trials, of which five candidates are in advanced clinical trials. For BNT111, an mRNA vaccine candidate for the treatment of advanced melanoma, we have received FDA fast track designation in the US. These designations are intended to facilitate and expedite the development of new drugs and vaccines for the treatment or prevention of serious diseases that have the potential to address unmet medical needs.
One of the challenges with personalized medicine, creating a specific treatment for one particular patient, is how to organize its official approval, since every patient gets a different product. Do you think we will need some legislative change there as well, or not necessarily?
Very early on, we started discussions with regulatory authorities. What is important, we believe, is that the process of manufacturing, and the mRNA backbone, stay the same. Within this frame, we just exchange the code for the cancer mutations.
The aim of such a framework would be that irrespective of the sequence of the mutations used to individualize a vaccine, if everything else stays the same, a complete approval process for an individualized version of the vaccine may not be required again, provided that the general product has been approved by the authorities for a certain tumor type. This is our aim, and I believe we are on the way to land there. This is new territory also for regulators, and we all need to learn.
Why has cancer been so difficult to cure, and is there a fundamental reason why you think mRNA vaccines could provide a way forward where other approaches haven’t?
The reason why cancer is so difficult is that it is a really complex disease. It is different in every person, and it shapeshifts over time. Because mRNA vaccines are versatile and can be manufactured on demand, we can personalize them. We can define the individual cancer fingerprint — its mutation profile — and design a specific vaccine to address these mutations.
And if the patient relapses because the cancer has changed, we can adapt the treatment accordingly, similar to how we are able to adapt our mRNA Covid-19 vaccines to new viral variants of concern.
The body does often produce immune cells that target a tumor. Why doesn’t it make the right ones — or enough of them — to suppress it? Why does it need help from a vaccine?
First of all, tumors have all sorts of tricks to suppress our immune cells, across the body but also within the tumor itself. In addition, many of the altered structures of the tumor are still recognized as part of the body, so they are tolerated by the immune system. Therefore, the ideal targets for the immune system are those in the tumor’s mutanome: the mutations that accumulate over time in cancer cells.
But only a tiny portion of those is recognized by spontaneously occurring, circulating T cells. With our mutation-based vaccine candidates, we aim to use the potential of the mutanome to help T cells get started.
Still, we find that we often need something to overcome the strong immune suppression from the tumor. These might be immune modulators such as immune checkpoint inhibitors, or chemotherapy, which results in the death of cancer cells, that can push the effect of a vaccine towards stronger activity.
One of the reasons you were able to act so fast when you realized that we had a pandemic on our hands was that in developing cancer vaccines, there is always time pressure, since an untreated tumor is growing every day. How far have you come in compressing development time, the time you need to get the vaccine into the patient, and how much further do you think you can go?
The process — starting with genome analysis of a patient’s tumor and ending with on-demand manufacturing of this customized mRNA vaccine ready to administer — has been a race against that specific patient’s growing tumor. Since 2014, we’ve made custom vaccines for hundreds of cancer patients in our clinical trials and shipped them worldwide. Back then, the process took us three to five months for each patient. Now we are at three to six weeks, and I would expect that we’ll become stable around three weeks at some point.
Do you think mRNA cancer vaccines will eventually be able to help everyone? Or are there some tumors that will always be out of reach?
In principle, we expect that cancer vaccines can be used universally, as there is currently no reason why there should be a tumor type that would not be approachable by this concept.
Having said that, I want to make clear that it would be a very romanticized view to think that we’ll have a cancer vaccine that will solve all problems. Again, cancer is a very complex disease.
However, cancer vaccines may be a potent option in the future that could complement the therapy toolkit and help to better treat patients with cancer.
10.1146/knowable-052523-2
TAKE A DEEPER DIVE | Explore Related Scholarly Articles




